The techniques used to deliver photon-based radiotherapy have advanced over the years, from 3D conformal radiotherapy, to intensity-modulated radiotherapy (IMRT) and volumetric-modulated arc therapy (VMAT). Each progression aims to confer higher conformality, faster delivery and increased plan robustness. Proton therapy technology has also evolved, from passive scattering to scanned pencil beams and intensity-modulated proton therapy (IMPT). But what’s next?
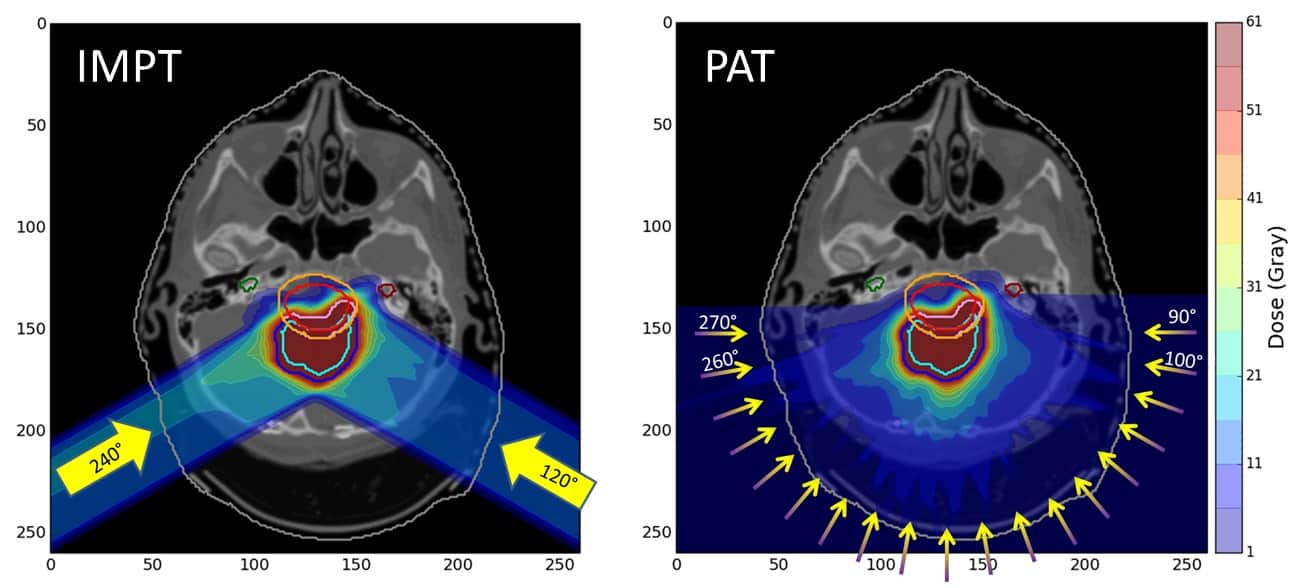
According to Yunzhou Xia from the University of Manchester, the next evolution in proton delivery is proton arc therapy (PAT). “Arc therapy is treatment with the radiation continuously on as the gantry rotates around the patient,” she explained. “It is different to IMPT, where the beam is switched off between gantry movements.” Unlike VMAT, however, PAT has only been studied since 2016 and is not yet part of routine clinical practise.
Speaking at the recent Medical Physics & Engineering Conference (MPEC), Xia described how the Bragg peak could make proton treatments sensitive to range uncertainties and set-up errors, and suggested that the greater number of control points in PAT compared with IMPT might increase the robustness of PAT treatment plans to uncertainties.
To assess the potential benefits of this approach, Xia created IMPT and PAT plans for one brain cancer and two head-and-neck cancer cases, with equivalent prescriptions for each pair of plans. She simulated range errors in the plans, including +/-3% over/undershoot and set-up errors of up to 3 mm in all directions. She then evaluated the dose distribution of each plan.
Xia first showed the audience the dose distributions for the brain tumour case, an ependymoma, for error-free IMPT and PAT plans. “In terms of target coverage, the two plans are very similar,” she said. “In the medium dose region, PAT delivers a more conformal dose to the target. However, in the lower dose region, PAT has more coverage.”
She then presented the values of conformity index (CI) and homogeneity index (HI) – tools used to quantitatively assess treatment plan quality – for pairs of plans with various uncertainties. PAT resulted in improved CI and HI values (closer to 1), for both range and set-up errors. This finding demonstrates that, for the ependymoma case, the PAT plans were more robust to errors than respective IMPT plans.
For the unilateral head-and-neck case, Xia showed that with no errors present, the PAT plan exhibited higher conformality and spared parts of the parotid gland compared with the IMPT plan. For plans with range errors, the CI and HI values were better with PAT than for IMPT, but PAT performed less well in plans with set-up errors.
Finally, Xia showed a bilateral head-and-neck case, with two target volumes: the first with a higher dose prescription than the second. Again, in the error-free instance, the PAT plan showed higher conformality than the IMPT version.
For the second, lower-dose, head-and-neck target, HI and CI values were closer to 1 for PAT plans than for IMPT, under both range and set-up errors. For the higher-dose target, CI was improved in the PAT plan while HI was better in the IMPT plan.
“Proton arc therapy has the potential to improve target robustness for certain brain and head-and-neck cases,” Xia concluded. “The narrower distribution of metrics in some cases may be beneficial for robust optimization.” Xia now plans to repeat this analysis using more cases in order to draw a statistical conclusion.