Researchers in the Netherlands have imaged the flow of blood in a living organism for the first time using a medical technology known as magnetic particle imaging (MPI). In the method, iron oxide nanoparticles were injected into the bloodstream of mice before their flow was traced through vital organs using a technique similar to magnetic resonance imaging (MRI).
If the technology can now be adapted for use in the human body it could be help to diagnose heart disease and cancer and to monitor the body’s reaction to the treatment of these conditions.
“If we can know the amount of blood absorbed by a cancerous tumour we can learn a lot about how it is reacting to particular treatments,” said Joern Bogert, one of the researchers at the Royal Phillips Research Lab in Hamburg.
Magnetic idea
Over the years, medical imaging procedures like X-ray and MRI have been honed to produce high quality snapshots of bones and hard tissue inside the body. When it comes to resolving softer tissues and fluids, however, these techniques have had limited success. However, iron oxide particles injected into the body are highly visible because there are no other naturally occurring magnetic particles in the blood stream.
After conceiving the technique of MPI in 2001, the Philips researchers then presented an initial set up of their MPI scanner in a Nature Paper of 2005. At that time MPI could only produce images in 2D and the processing times were far too slow to be useful for medical applications.
Over the past four years, the researchers have improved the technique to obtain high spatial resolutions in 3D, and images can be captured over time periods as short as one fiftieth of a second.
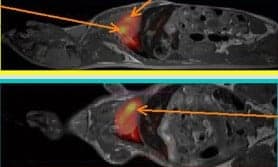
With this latest advance, the researchers have transferred MPI from an inorganic demonstration to a full preclinical trial in a live organism. The series of in vivo experiments comprised scans on 18 mice using tracer concentrations in the range between 8 and 45 micro moles of iron oxide. To confirm that the MPI signal truly reflected the anatomy of the mice, the researchers then transferred the mice to a standard MRI scanner and produced a series of reference images (Phys. Med. Biol. 54.5).
Hospital-ready?
“Testing MPI in vivo is a major breakthrough for us – bodies are incredibly complex and that’s why so many new medical procedures fail at this stage,” Bogert told physicsworld.com
The next step is to scale up this technique for use on humans. Using a range of scaling factors, the researchers predict that – without any further enhancement to the technique – it would produce images that are only 10 per cent as good as those from the mice experiments. Given this drawback, this new technology may still be a long way from making it into hospitals.
“MPI may be able to replace or compliment some MRI procedures, but it’s not likely that it would replace MRI altogether,” said Philip Grandinetti an NMR methods researcher at Ohio State University.”
Matthew Allen of Wayne State University is also cautious. “MPI may be useful for imaging functions like coronary blood supply but MRI gives anatomical data that MPI cannot – because MRI images tissue not nanoparticles.”
“Other hurdles might include obtaining approval from the government for the use of MPI in the clinic and convincing doctors to switch from their current imaging techniques to MPI,” he added.



