Diagnosing a brain tumour usually entails neuroimaging with CT and MRI, followed by surgical resection or tissue biopsy. A non-invasive and inexpensive alternative is blood-based liquid biopsy, which analyses circulating biomarkers in the blood to obtain molecular and genetic information about the tumour and guide treatment decisions. Unfortunately, brain tumour-derived biomarkers are detected only in scarce amounts, as the blood–brain barrier (BBB) prevents the transfer of such biomarkers into the peripheral circulation.
To address this problem, researchers at Washington University in St. Louis are using focused ultrasound (FUS) and microbubbles to temporarily disrupt the BBB and release large amounts of biomarkers into the bloodstream for analysis. In a first-in-human prospective trial, they found that FUS-induced release of biomarkers into the bloodstream – a method they call sonobiopsy – is feasible and safe for use.
“With this technique, we can obtain a blood sample that reflects the gene expression and the molecular features at the site of a lesion in the brain. It’s like doing a brain biopsy without the dangers of brain surgery,” explains co-senior author Eric Leuthardt in a press statement.
Transcranial low-intensity FUS, used in combination with intravenously injected microbubbles, provides temporal and reversible opening of the BBB and can target lesions in the brain with millimetre accuracy. The microbubbles, which are traditionally used as ultrasound contrast agents, undergo cavitation upon exposure to FUS and amplify its mechanical effects.
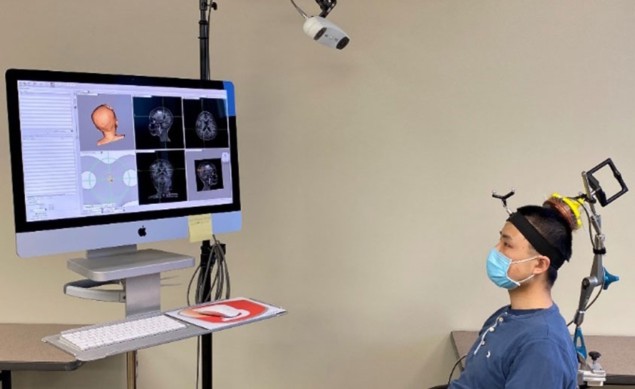
To perform sonobiopsy, a technique pioneered by Leuthardt and co-senior author Hong Chen, the team developed a compact FUS device that can be directly attached to a clinical neuronavigation probe, enabling precise positioning of the FUS transducer. This design enables easy integration of sonobiopsy into existing clinical workflows without requiring neurosurgeons to undertake additional training.
To assess the feasibility and safety of sonobiopsy with the neuronavigation-guided FUS transducer, Leuthardt, Chen and colleagues carried out a pilot single-arm trial of five patients with high-grade glioma (four had glioblastoma, one had a diffuse high-grade glioma).
The researchers performed sonobiopsy on anaesthetized patients prior to planned surgical brain tumour removal. Using MRI and CT images acquired beforehand to register the patient’s head position, they positioned the FUS transducer to align its focus at the tumour location. After intravenous injection of microbubbles, they applied FUS sonication for 3 min.
Analysis of blood samples collected before and 5, 10 and 30 min after sonication revealed that sonobiopsy increased the concentration of circulating tumour DNA (ctDNA). This included maximum increases of 1.6-fold for mononucleosome cell-free DNA (cfDNA) fragments, 1.9-fold for patient-specific tumour variant ctDNA, and 5.6-fold for ctDNA with TERT mutations (which are present in more than half of glioblastoma patients and associated with poor treatment outcomes).
The study also verified that the procedure was safe and did not damage brain tissue. During FUS sonication, patients did not exhibit any significant fluctuations in vital signs and there were no adverse events. Tumour samples collected during surgery showed no microhaemorrhage or structural changes between sonicated and non-sonicated regions.
Ultrasound implant helps deliver powerful chemotherapy to brain tumours
The researchers conclude that their work “marks a crucial initial milestone in demonstrating the feasibility and safety of sonobiopsy in patients with high-grade glioma”. They point out that while this study was performed in an operating room prior to surgery, operative environments and anaesthesia are not essential, and sonobiopsy could be used in a clinic or at a patient’s hospital bedside.
“With this capability to non-invasively, non-destructively access every part of the brain, we can now obtain genetic information from tumours at every stage of patient care, ranging from tumour diagnosis to treatment monitoring and detection of recurrence,” says Chen. “We can now start to interrogate diseases that traditionally don’t undergo surgical biopsies, such as neurodevelopmental, neurodegenerative and psychiatric disorders.”
The study is described in npj Precision Oncology.




