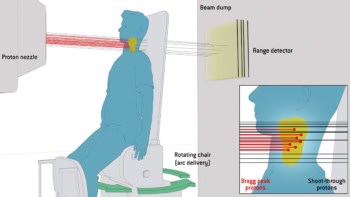
Proton therapy can deliver superior dose distributions compared with photon-based radiotherapy, enabling radiation oncologists to precisely target a tumour while reducing the risk of damage to adjacent healthy tissue. Pencil-beam scanning (PBS), the most advanced type of proton therapy, increases this precision by shaping the delivered radiation to a tumour’s exact volume. A team at the West German Proton Therapy Centre Essen (WPE) has now shown that the addition of static apertures to PBS treatments further reduces the dose to nearby normal tissue while maintaining the target dose.
The pencil beams used in PBS proton therapy typically have a spot size of 1 cm (full-width at half maximum) or more, which can impede the sparing of organs-at-risk adjacent to the target volume. The dose fall-off in the lateral direction also limits the options for covering the target while keeping dose to normal tissue at tolerable levels. The WPE team demonstrated that using static apertures to trim these spot-scanning fields reduced the dose to organs-at-risk such as the eye lens and brainstem, and in six brain tumour cases reduced the dose to the brain and hippocampi.
Static apertures enable small air gaps in clinical treatment plans, which is beneficial for the lateral dose gradient. At some proton therapy centres, static apertures are a standard piece of equipment. At WPE, the research team fabricated brass apertures for each individual treatment field using a computerized milling machine. The actual number of apertures used was optimized per treatment field to achieve efficient production and treatment workflow.

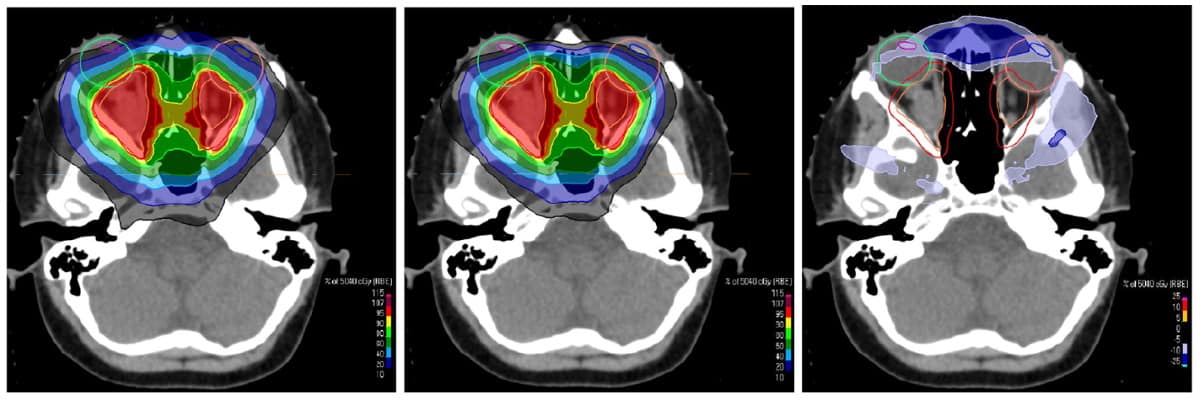
Writing in Frontiers in Oncology, Christian Bäumer and colleagues report that “uncollimated” treatment plans for 31 patients with various brain cancers were prepared for conventional PBS delivery. The researchers then inserted apertures for all fields, specifying a lateral margin for the planning target volume (PTV) coverage and blocking adjacent organs-at-risk. They adapted margins for each individual field, and chose the number of fields and their arrangement based on the location of the target.
Quality assurance procedures for treatment plans needed to be modified from the centre’s established procedures to align the X-ray imaging, PBS and aperture systems. The researchers caution that the positioning of the aperture relative to the PBS field is impacted by movement of the snout (the part of the proton delivery nozzle closest to the patient) and the aperture mounting mechanism. The team also performed a robustness evaluation based on perturbed dose scenarios to account for possible deviations of the centre of the pencil beam and the mechanical centre of the aperture holder.
The researchers assessed the dosimetric benefits of the 31 treatment plans delivered using apertures compared with the corresponding plans without apertures. “The volume of the dose gradient surrounding the PTV (evaluated between 80% and 20% dose levels) was decreased on average by 17.6%,” they write. “For the full cohort of 31 cases, the mean brain dose could be reduced on average by 1.2 Gy(RBE) through apertures.”
The most noticeable improvement, they note, was a reduction in dose to the hippocampi of between 1.6 and 4.7 Gy(RBE), with a mean decrease of 2.9 Gy(RBE).

The study included six cases of the brain tumour craniopharyngioma, with targets located near important organs-at-risk including the brainstem, optic nerves, chiasma and hippocampi. The biggest benefit of using PBS with static apertures was achieved for the thalamus, brainstem and hippocampus, where the mean doses were reduced by 5.5, 5.6 and 3.1 Gy(RBE), respectively. For two cases, the mean dose to the eye lens was reduced to below 5 Gy(RBE), which could not have been achieved without using apertures.
In all 31 cases, the dose burden to normal tissue was reduced and the dose target maintained when apertures were used. In four cases, the dose to organs-at-risk was reduced to a level below the tolerance dose, which could only be achieved with the use of the static apertures.
The authors point out that their study was limited to a horizontal beam line. They expect further dosimetric benefits if a gantry is available for the proton treatment. “In the future, we expect an even better dose sparing of normal tissue through the use of dynamic adaptive collimators, which have not yet been clinically released,” says Bäumer.