Stereotactic ablative radiotherapy (SABR) is a popular method for treating small, inoperable tumours in various anatomical sites. This type of radiotherapy delivers highly focused, intense radiation doses in few treatment sessions, which increases the radiation’s cell-killing effectiveness. A phase II study conducted by researchers from the Johns Hopkins Sidney Kimmel Cancer Center has now shown that SABR can slow disease progression in prostate cancer patients with up to three metastases (JAMA Oncol. 10.1001/jamaoncol.2020.0147).
Prostate cancer is the second most common cancer in men worldwide and the most common in the USA and many European countries. Once the tumour has metastasized, the disease is incurable, though treatment options exist that can slow its progression. One standard treatment for men with hormone-sensitive metastatic prostate cancer is a type of hormone therapy called androgen deprivation therapy (ADT). However, ADT can have side effects such as impotence or loss of bone and muscle density. Many men therefore prefer to delay this treatment for as long as possible.
SABR as an alternative to early hormone therapy
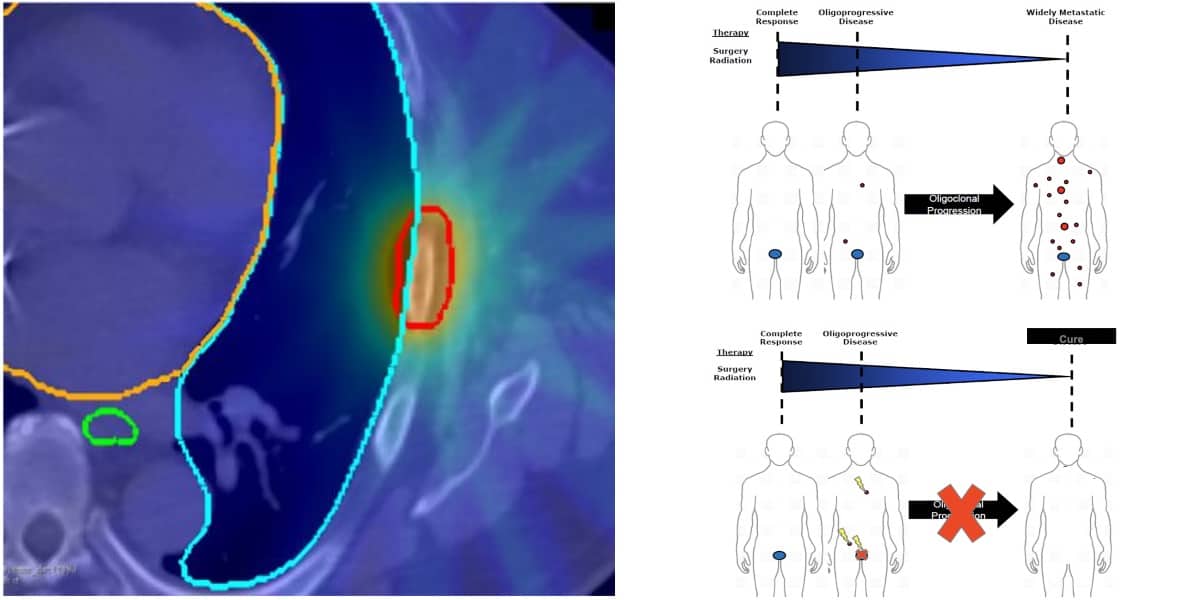
Recently, SABR has been gaining interest as a treatment option for cancers in the early metastatic (oligometastatic) stage, where patients have few, localized metastases. The results of the ORIOLE (Observation versus Stereotactic Ablative Radiotherapy for Oligometastatic Prostate Cancer) phase II randomized controlled trial suggest that treating prostate cancer oligometastases with SABR early on could be a strategy to delay the need for ADT and its harsh side effects.
The trial included 54 men with recurrent hormone-sensitive prostate cancer, and between one and three metastases, who were randomized to receive either SABR or observation only.

The researchers, led by Phuoc Tran of the Johns Hopkins University School of Medicine, report that of 36 patients treated with SABR only, seven (19%) suffered disease progression after six months, while 11 of 18 (61%) in the observation-only group did. Tran and colleagues further report no severe side effects in the SABR trial arm and no significant difference in patient-reported quality-of-life when compared with the observation-only arm.
Triggering the immune system
In addition to showing SABR’s safety and effectiveness for treating these patients, the ORIOLE trial results also hint at an underlying mechanism. The researchers detected an expanded population of T cells in the blood of patients treated with SABR compared with observation-only patients. This suggests that the treatment may have stimulated a body-wide immune response towards the tumours.
“It has been a longstanding question, especially important now in the era of immunotherapy, whether any type of radiation, and SABR specifically, can stimulate the immune system,” Tran said in a recent press release. “Our trial offers the best data to date to suggest that SABR can cause a systemic immune response.”
Finally, the team found that the patients could be divided into low-risk and high-risk groups based on specific tumour gene mutations. They found that SABR was especially effective at slowing disease progression in the low-risk group, indicating that tumour DNA mutation profiles might predict how well a patient responds to SABR.
While these results point to exciting possibilities for new combined treatments and patient risk stratification, Tran and colleagues caution that further studies are needed to validate these insights. Currently, the team is focusing its efforts on further investigating disease-slowing treatments for metastatic cancers. For example, in an ongoing trial called RAVENS, they examine the effect of combining SABR with radium-223 to combat bone metastases.