Medical physics techniques play a key role in all areas of cardiac medicine – from the use of advanced imaging methods and computational modelling to visualize and understand heart disease, to the development and introduction of novel pacing technologies. At a recent meeting organised by the Institute of Physics’ Medical Physics Group, experts in the field discussed some of the latest developments in cardiac imaging and therapeutics, with a focus on transitioning technologies from the benchtop to the clinic.
Monitoring metabolism
The first speaker, Damian Tyler from the University of Oxford described how hyperpolarized MRI can provide “a new window on the reactions of life”. He discussed how MRI – most commonly employed to look at the heart’s structure and function – can also be used to characterize cardiac metabolism, with metabolic MR studies helping us understand cardiovascular disease, assess drug mechanisms and guide therapeutic interventions.
In particular, Tyler is studying pyruvate, a compound that plays a central role in the body’s metabolism of glucose. He explained that 13C MR spectroscopy is ideal for studying pyruvate metabolism, but its inherent low signal-to-noise ratio makes it unsuitable for rapid in vivo imaging. To overcome this limitation, Tyler uses hyperpolarized MR, which increases the sensitivity to 13C-enriched tracers by more than 10,000 times and enables real-time visualization of normal and abnormal metabolism.
As an example, Tyler described a study using hyperpolarized 13C MR spectroscopy to examine cardiac metabolism in diabetes, which is associated with an increased risk of heart disease. Tyler and his team examined the downstream metabolites of 13C-pyruvate (such as 13C-bicarbonate and 13C-lactate) in subjects with and without type 2 diabetes. They found reduced bicarbonate levels in diabetes and increased lactate, noting that the bicarbonate to lactate ratio could provide a diagnostic marker.
Among other potential clinical applications, hyperpolarized MR could be used to detect inflammation following a heart attack, elucidate the mechanism of drugs and accelerate new drug discovery, and provide an indication of whether a patient is likely to develop cardiotoxicity from chemotherapy. It can also be employed to guide therapeutic interventions by imaging ischaemia in tissue and assess cardiac perfusion after heart attack.
“Hyperpolarized MRI offers a safe and non-invasive way to assess cardiac metabolism,” Tyler concluded. “There are a raft of potential clinical applications for this emerging technology.”
Changing the pace
Alongside the introduction of new and improved diagnostic approaches, researchers are also developing and refining treatments for cardiac disorders. One goal is to create an effective treatment for heart failure, an incurable progressive condition in which the heart can’t pump enough blood to meet the body’s needs. Current therapies can manage symptoms, but cannot treat the underlying disease or prevent progression. Ashok Chauhan from Ceryx Medical told delegates how the company’s bio-inspired pacemaker aims to address this shortfall.
In healthy hearts, Chauhan explained, the heart rate changes in response to breathing, in a mechanism called respiratory sinus arrythmia (RSA). This natural synchronization is frequently lost in patients with heart failure. Ceryx has developed a pacing technology that aims to treat heart failure by resynchronizing the heart and lungs and restoring RSA.

The device works by monitoring the cardiorespiratory system in real time and using RSA inputs to generate stimulation signals in real time. Early trials in large animals demonstrated that RSA pacing increased cardiac output and ejection fraction compared with monotonic (constant) pacing. Last month, Ceryx begun the first in-human trials of its pacing technology, using an external pacemaker to assess the safety of the device.
Eliminating sex bias
Later in the day, Hannah Smith from the University of Oxford presented a fascinating talk entitled “Women’s hearts are superior and it’s killing them”.
Smith told a disturbing tale of an elderly man with chest pain, who calls an ambulance and undergoes electrocardiography (ECG) that shows he is having a heart attack. He is rushed to hospital to unblock his artery and restore cardiac function. His elderly wife also feels unwell, but her ECG only shows slight abnormality. She is sent for blood tests that eventually reveal she was also having a severe heart attack – but the delay in diagnosis led to permanent cardiac damage.
The fact is that women having heart attacks are more likely to be misdiagnosed and receive less aggressive treatment than men, Smith explained. This is due to variations in the size of the heart and differences in the distances and angles between the heart and the torso surface, which affect the ECG readings used to diagnose heart attack.
To understand the problem in more depth, Smith developed a computational tool that automatically reconstructs torso ventricular anatomy from standard clinical MR images. Her goal was to identify anatomical differences between males and females, and examine their impact on ECG measurements.
Using clinical data from the UK Biobank (around 1000 healthy men and women, and 84 women and 341 men post-heart attack), Smith modelled anatomies and correlated these with the respective ECG data. She found that the QRS complex (the signal for the heart to start contracting) was about 6 ms longer in healthy males than healthy females, attributed to the smaller heart volume in females. This is significant as it implies that the mean QRS duration would have to increase by a larger percentage for women than men to be diagnosed as elevated.
She also studied the ST segment in the ECG trace, elevation of which is a key feature used to diagnose heart attack. The ST amplitude was lower in healthy females than healthy males, due to their smaller ventricles and more superior position of the heart. The calculations revealed that overweight women would need a 63% larger increase in ST amplitude to be classified as elevated than normal weight men.
Smith concluded that heart attacks are harder to see on a woman’s ECGs than on a man’s, with differences in ventricular size, position and orientation impacting the ECG before, during and after heart attacks. Importantly, if these relationships can be elucidated and corrected for in diagnostic tools, these sex biases can be reduced, paving the way towards personalised ECG interpretation.
Prize presentations
The meeting also included a presentation from the winner of the 2023 Medical Physics Group PhD prize: Joshua Astley from the University of Sheffield, for his thesis “The role of deep learning in structural and functional lung imaging”.
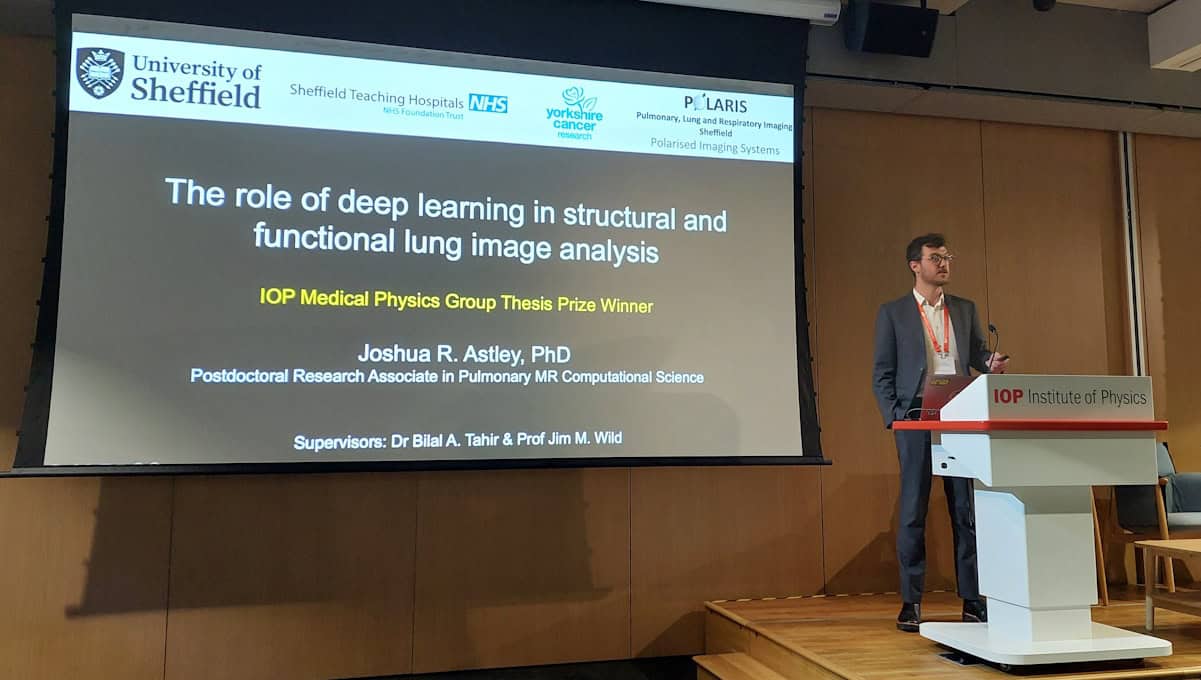
Shifting the focus from the heart to the lungs, Astley discussed how hyperpolarized gas MRI, using inhaled contrast agents such as 1He and 129Xe, can visualize regional lung ventilation. To improve the accuracy and speed of such lung MRI studies, he designed a deep learning system that rapidly performs MRI segmentation and automates the calculation of ventilation defect percentage via lung cavity estimates. He noted that the tool is already being used to improve workflow in clinical hyperpolarized gas MRI scans.
Astley also described the use of CT ventilation imaging as a potentially lower-cost approach to visualize lung ventilation. Combining the benefits of computational modelling with deep learning, Astley and colleagues have developed a hybrid framework that generates synthetic ventilation scans from non-contrast CT images.

Dynamic nuclear polarization: how a technique from particle physics is transforming medical imaging
Quoting some “lessons learnt from my thesis”, Astley concluded that artificial intelligence (AI)-based workflows enable faster computation of clinical biomarkers and better integration of functional lung MRI, and that non-contrast functional lung surrogates can reduce the cost and expand use of functional lung imaging. He also emphasized that quantifying the uncertainty in AI approaches can improve clinician’s trust in using such algorithms, and that making code open and available is key to increasing its impact.
The day rounded off with awards for the meeting’s best talk in the submitted abstracts section and the best poster presentation. The former was won by Sam Barnes from Lancaster University for his presentation on the use of electroencephalography (EEG) for diagnosis of autism spectrum disorder. The poster prize was awarded to Suchit Kumar from University College London, for his work on a graphene-based electrophysiology probe for concurrent EEG and functional MRI.