The ability to assess the impact of radiation on malignant tumours during a course of radiotherapy could help improve its effectiveness for individual patients. Based on tumour response, physicians could modify the treatment regimen, dose and radiation field accordingly.
Israeli researchers have now demonstrated that thermography may provide a viable radiotherapy monitoring tool for such treatment optimization. They have developed a method to detect tumours in a thermal image and estimate changes in tumour and vasculature during radiotherapy, validating this in a study of six patients with advanced breast cancer (J. Biomed. Opt. 23 058001).
Thermography had been rejected as a breast cancer detection tool, due to its suboptimal sensitivity and specificity. However, for an already detected tumour undergoing radiation or chemotherapy, it could prove a highly effective monitoring tool, when incorporating algorithms developed by the research team.
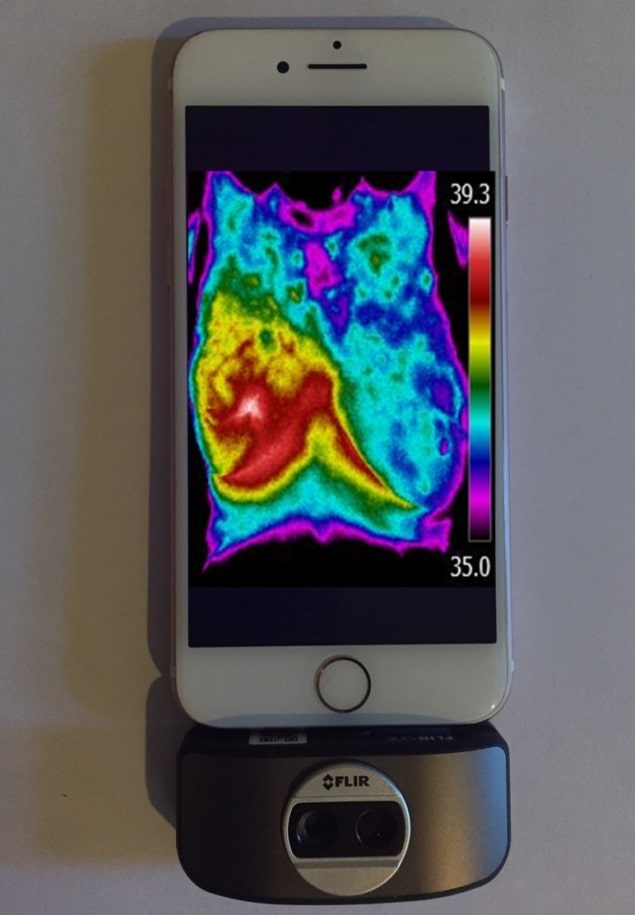
The multi-institutional team had conducted research on thermal imaging to understand tumour aggressiveness in animal models. They hypothesized that because malignant tumours are characterized by abnormal metabolic and perfusion rates, they will generate a different temperature distribution pattern compared with healthy tissue. By measuring skin temperature maps at the tumour location before and during treatment, the reaction of a tumour to radiotherapy can be measured.

Israel Gannot from Tel-Aviv University and co-authors developed a four-step algorithm to analyse the thermal images. First, images were converted from colour to grey scale and a fixed temperature range of 7°C set for all images, to enable comparison of the entropy (which characterizes the homogeneity of the image) in different images. Images were filtered using a Frangi filter designed to emphasize tubular structures. This filter highlighted blobs of heat (the malignant tumour) and long, narrow tubular objects (the blood vessel network). Images were enlarged sevenfold to observe local temperature changes in the blood vessels.
In the final step, feature extraction, the algorithm calculates entropy in the cropped thermal image of the tumour area and in the filtered tumour image. It then estimates changes in tumour regularity and vasculature shape during radiotherapy.
Patient imaging
The six patients were women with stage IV breast cancer and distant metastatic disease. None had undergone surgical resection of their tumours, which had a diameter larger than 1 cm at a depth of less than 1 cm. All patients received 15 radiation fractions of 3 Gy, administered over three weeks.
The patients underwent thermal imaging before each radiotherapy session and a day after the end of the session. Room temperature and humidity were controlled during image acquisition and fluorescent lights were turned off. The thermal camera, positioned 1 m from the patient, acquired images containing either 320×256 or 320×240 pixels.
The authors report that entropy was reduced in the tumour areas, for all patients, during radiation treatment. They described the appearance of the tumour vasculature as “a crab with many arms”. To quantify changes in the shape of vascular networks, they converted the images into binary images and counted the number of objects before and after radiotherapy. They saw a reduction in the number of objects, indicating a reduction in the vessels supplying nutrients to the tumour.
Expanding applications
The researchers selected breast cancer for the initial research because co-researcher Merav Ben-David, from Sheba Medical Center, specializes in breast cancer treatment. They are now looking at additional applications, such as the treatment of cervical cancer and head-and-neck cancer.
“We are collecting more data to run big data statistics,” Gannot tells Physics World. “We are also starting to implement the use of this technology as a tool for early warning of breast cancer by women at their home, using a thermal camera attached to a cell phone with our algorithms implemented in the smartphone app. This is intended for use in addition to mammography. It could fill the time span between mammography examinations when many cancers develop.”
In future research, the authors are planning to use thermal imaging devices with multiple angles and perform real-time analysis. They are planning larger studies to evaluate the efficacy of thermography to monitor radiotherapy, chemotherapy and immunotherapy treatments.