As tumours progress and grow, they undergo mechanical alterations such as changes in extracellular matrix rigidity and build-up of compressive stress. A European research team has now proposed that this compression of solid tumours may help explain why some cancers are resistant to chemotherapy drugs.
To test their hypothesis, the researchers examined tumour spheroids formed from pancreatic cancer cells. Under normal free-growth conditions, the spheroids increased in size to reach diameters of hundreds of microns. They also embedded spheroids in agarose gel. This confinement reduced cell proliferation, slowed the spheroid growth and after a few days, led to growth-induced pressure in the kilopascals range.
“We chose to work on pancreatic cancer because it is both one of the deadliest cancers, and one where the impact of compressive stress is very important, as pancreatic tumours are highly compressed,” explains Morgan Delarue from LAAS-CNRS. “We chose to examine the link between mechanical stress and chemotherapy efficacy.”
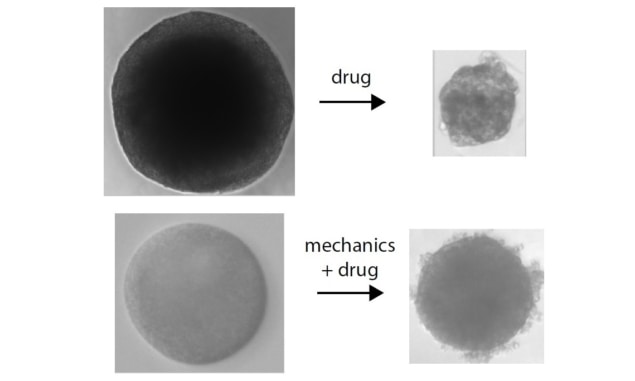
In a study described in Physical Review Letters, Delarue and colleagues – also from HZI, Claude Bernard Lyon 1 University and CRCT – treated both types of spheroid with 10 μM of the chemotherapy drug gemcitabine. They found that compressed spheroids were less sensitive to the drug than freely growing ones. The unconfined spheroids decreased in size by 30–40% after drug exposure, while spheroids treated after two days of confined growth shrank by less than 10%.
As gemcitabine targets proliferating cells, this reduced drug efficacy under compression may well be due to the decrease in cell proliferation. However, compression could also trigger mechanosensitive pathways that act directly on the drug, such that it does not reach the cells, is exported out of the cells or de-activated by the cell, for example.
To explore these potential mechanisms, the researchers developed a mathematical model to predict the combined effect of compression and drug exposure on spheroid growth. The model made two assumptions: that cell growth rate is affected by pressure; and that the drug only kills proliferating cells, with a killing rate that does not depend on pressure.
“We could not selectively test all these parameters experimentally, so we opted for a mathematical model with just two ingredients,” Delarue explains. “We can calibrate both parameters independently: proliferation under pressure, and drug killing without pressure. We also assumed a linear coupling between growth and drug-induced death.”
The model accurately predicted the experimental data – implying that tumour resistance arises solely from the effect of compression on cell proliferation. “We observed an outstanding prediction,” says Delarue. “This strongly suggests the aforementioned mechanism, as other impacts of the mechanics on the drug would not be predicted by this model.”
This interpretation also implies that lowering compressive stress should increase cell proliferation and thus improve drug efficacy. To test this, the researchers examined gel-embedded spheroids treated over 6–7 days, after which time they had decreased in size such that they were no longer compressed. The model captured the experimental data exactly: a slow initial death velocity during compression, followed by a faster one in the unconfined phase.
This mechanical form of drug resistance should be independent of the type of drug used and the type of mechanical stress applied. The researchers confirmed both of these predictions. Firstly they treated spheroids with a different chemotherapeutic, docetaxel. The model accurately predicted the experimental results, with docetaxel efficacy reduced in compressed spheroids.
They next applied a different kind of mechanical stress: osmotic compression with dextran. Osmotically compressed spheroids treated with gemcitabine showed a similar modulation of drug efficacy as seen with growth-induced pressure. Again, the model accurately predicted these effects, further reinforcing the premise that mechanics decreases drug efficacy by modulating cell proliferation.
The team is continuing to work on this question of how compressive stress impacts cancer progression and treatment. “Additionally, we are seeking to understand how exactly compressive stress plays a role on cell proliferation,” Delarue tells Physics World. “We know it stops proliferation, but how? Understanding this point would help us to develop coupled therapies: a drug which would force cells to proliferate under pressure, plus a chemotherapeutic to kill them.”



