Ultrasound elastography can be used to diagnose kidney disease, providing a more reliable estimate of impairment than methods based on blood tests or kidney dimensions. Sook Sam Leong and colleagues at the University of Malaya in Kuala Lumpur measured Young’s modulus derived from shear wave elastography in the kidneys of patients undergoing accurate but expensive radiotracer-based tests, and found that they correlated negatively with renal function. The technique also indicated which kidney was dominant — an important determination for kidney donors undergoing transplant surgery (Ultrasound Med. Biol. 10.1016/j.ultrasmedbio.2019.01.024).
Chronic kidney disease (CKD) is defined as a persistently low glomerular filtration rate (GFR) — the rate at which blood plasma is filtered by the kidneys. Combined GFR for both kidneys can be assessed by injecting into the patient a water-soluble salt labelled with radioactive chromium-51 (51Cr-EDTA), and measuring the level of radioactivity in a blood sample drawn a few hours later.
Another radiotracer also delivered intravenously — technetium-99m-labelled dimercaptosuccinic acid (99mTc-DMSA) — is used to indicate the relative function of each individual kidney. In this technique, a GFR difference between the two organs is revealed by images captured using a gamma camera several hours after the radiotracer is administered.
“Currently, these two tests are the gold standard diagnostic procedures in assessing renal function,” says Kwan Hoong Ng, who led the research team. Unfortunately, not all clinics have access to nuclear medicine, and even where the techniques are available, they cannot always be used. The problem, says Ng, is that “they are time-consuming, they involve radiation exposure and, most importantly, they are expensive.”
A cheaper and quicker way of estimating GFR is to measure more accessible proxies, such as the level of muscle breakdown products in the blood, ultrasound echogenicity of the kidney as a whole, and even the organs’ lengths and volumes. None of these approaches are especially accurate, however, and all of them have been shown to be potentially insensitive to some indicators of serious renal disease.
Seeking a diagnostic technique that is simultaneously sensitive, affordable and convenient, Leong and colleagues found an alternative proxy in the changing tissue properties that accompany decreasing kidney function. Biopsies have shown that, as renal disease progresses, deposition of fibrous scar tissue in the kidneys leads to stiffening. Previous studies appeared to find that this stiffening was reflected in increased kidney shear wave velocity, but these mechanical changes were compared to estimates of GFR made using possibly unreliable means, rather than the radiotracer-based gold standard.
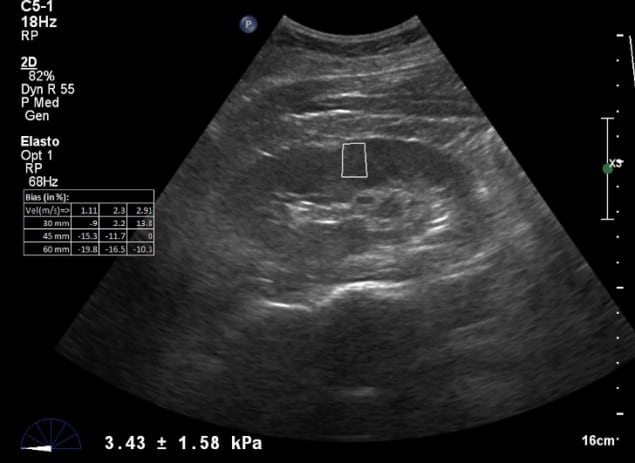
To address this uncertainty, the researchers used ultrasound to measure Young’s modulus and shear wave velocity within a sub-volume of the kidneys of 57 patients who also underwent 51Cr-EDTA-based GFR measurement and 99mTc-DMSA scintigraphy-based measurement of relative kidney function.

OCT could help expand the kidney donor pool
The results confirmed that shear wave elastography-based measurements of Young’s modulus and shear wave velocity can be used as a quick and easy diagnostic tool for kidney disease, and that they can identify an imbalance in function between the two kidneys in a given patient. The link between tissue stiffness and disease is still not completely clear-cut, however, as some research has suggested the opposite relationship, with tissue stiffness correlated positively with GFR.
“Two studies suggested that kidney stiffness increases with kidney function due to increased blood flow,” says Ng. “The correlation was only made between stiffness and perfusion without histological parameters, so future works need to be done to include both the histological evaluation and blood perfusion.”
Although the results suggest that shear wave elastography could replace other proxy-based methods of estimating GFR — and perhaps even radiotracer-based procedures — the researchers caution that the technique is not yet ready for the clinic. “We are the first and the only centre exploring this method, so more research on this area should be conducted by other centres to confirm the results,” says Ng.



