A surgical catheter that can change its rigidity as needed during operations has been developed by researchers from Switzerland and Spain. The tool – the core of which is built from a tailored phase-change alloy – could improve the safety of minimally-invasive ophthalmic surgeries.
One procedure that could benefit from such a tool is epiretinal membrane peeling, a delicate surgery that only highly skilled surgeons can perform. Epiretinal membranes are thin, transparent layers of fibrous tissues that can form over the retina and, in severe cases, cause one’s vision to become blurred and distorted. They most commonly arise in those aged 50 and older, as a result of age-related detachment of the vitreous jelly from the retina. However, the condition can also manifest following ocular surgery, inflammation of the eye or as a consequence of diabetic retinopathy. It is estimated that some 2% of people aged 50 or older – and 20% of 75-year-olds – have such membranes in one or both eyes, although treatment is usually only necessary in around 15% of cases.
Epiretinal membranes are removed in a surgical procedure that sees the pathological cell layer – which is typically some 60 µm thick – gently peeled off by a tiny, rigid gripping tool inserted into the eye. To reduce the risk of harming the sensitive retina, the operation starts with the vitreous being removed from the patient’s eye and replaced with a saline solution that is less susceptible to transferring potentially damaging shear forces. Nevertheless, the procedure still relies on the finely controlled application of force to avoid retinal tearing.
To minimize this risk further, medical roboticist Quentin Boehler of ETH Zurich and colleagues have developed a new type of catheter comprising a core made of a low melting point alloy (LMPA) that’s sandwiched, alongside a heating wire, between two insulating polymer layers. The device is just 1 mm thick in total.
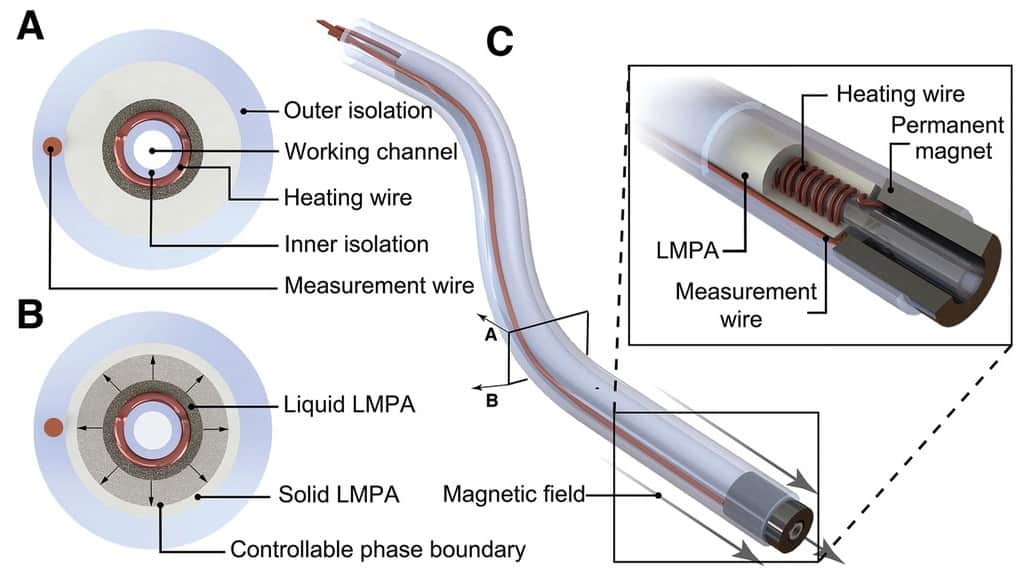
As its temperature rises, the alloy progressively melts from its core outwards, resulting in an increase in flexibility that can be reversed by allowing the catheter to cool back down. The alloy is tuned such that the phase transition occurs at 47°C – above the temperature of the human body (37°C), but not so high as to cause physiological damage.
A resistance-measuring wire contained in the catheter’s outer insulating layer allows operators to monitor the alloy temperature and, by extension, ensure the desired liquid-to-solid ratio and corresponding rigidity. In this way, the catheter – which has a magnetic tip – can be safely navigated, by an external magnetic field, to its desired target in its soft state before being allowed to stiffen in order to deliver the desired force to the pair of grippers at its end.
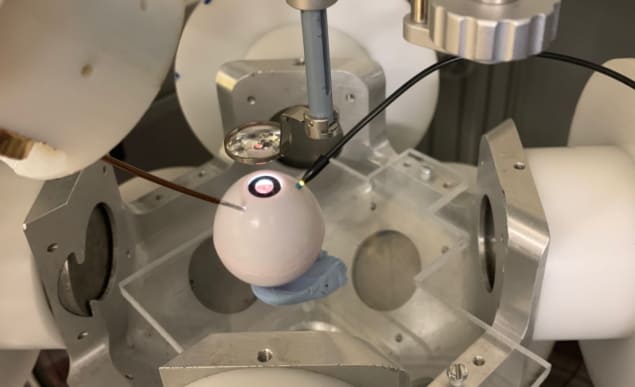
According to the team, the wire takes approximately 16 s to heat to a fully flexible state under surgical conditions and some 30 s to cool back down, and can deliver forces that range from 20 mN to 8 N. To demonstrate the potential of the concept, the researchers successfully performed a simulated membrane peeling operation on an eyeball phantom, onto which they had pressed a thin Parafilm layer to simulate the unwanted cell layer.
“We believe that our approach simply provides much more safety to the procedure,” says Boehler, noting that the catheter can also be adapted into a microcannula to inject drugs behind the retina. “More generally, we believe that variable-stiffness soft continuum robots can be part of the next generation of minimally invasive medical tools using robotic assistance, as they will benefit from increased safety and dexterity provided by this feature.”
Flexible electronics make their way into the operating room
“While shape morphing instruments have been available in laparoscopic surgery for a while, at the submillimetre level at which eye surgery is performed such capabilities were until now not possible,” comments Marc de Smet, an ophthalmic surgeon from the MIOS Centre in Lausanne who was not involved in the present study. However, he added, the current time constants are “relatively long in the hands of a surgeon poised to carry out a task that might involve 60 s in a given position”.
Furthermore, he continued, “while a 1 mm diameter is considerable achievement, current vitreoretinal surgery is carried out at diameters of 0.63 mm or less. At 1 mm, sutures are required at the end of surgery to close the wound, while at 0.63 mm or less, suture-less surgery associated with rapid healing is possible.”
With this initial study complete, the researchers are moving to demonstrate their catheter in animal models, with the goal of delivering a human intervention in the near future.
The study is described in Advanced Science.