X-ray mammography is the standard modality used to screen for early signs of breast cancer., Superposition of tissue in 2D mammograms can, however, sometimes mask cancerous lesions. To improve lesion visibility, some early adopters have begun to use digital breast tomosynthesis (DBT) alongside mammography. But before its adoption in routine breast screening, DBT requires thorough evaluation under clinically relevant conditions.
To address this task, researchers from the University of Surrey and Royal Surrey County Hospital have performed a virtual clinical trial comparing the performance of DBT and 2D-mammography (Phys. Med. Biol. 63 095014).
“We have developed a set of validated tools that allow us to model the key processes of X-ray breast imaging and produce simulated digital mammograms and DBT images,” explained first author Premkumar Elangovan. “One of the advantages is that we can insert simulated cancers into simulated breast models under a variety of conditions. This allows us to explore a range of tightly controlled imaging conditions that would be difficult to replicate in a clinical trial involving human subjects.”
Detection tasks
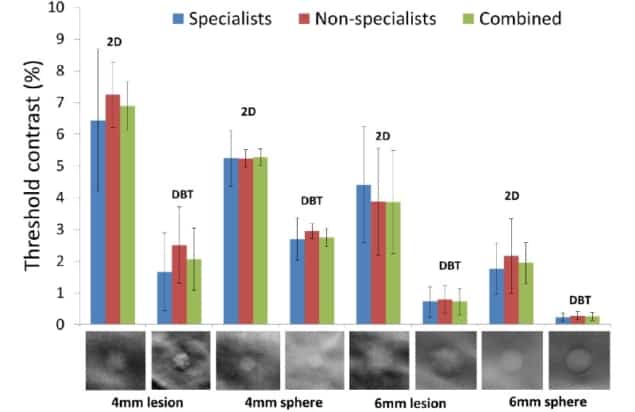
Elangovan and colleagues created 2D mammography and DBT projection images of virtual breast phantoms containing uniform spherical targets or solid masses with irregular margins. The targets had diameters of 4 or 6 mm, approaching the minimum detectable lesion size found in breast screening, and were simulated with three different contrast levels.
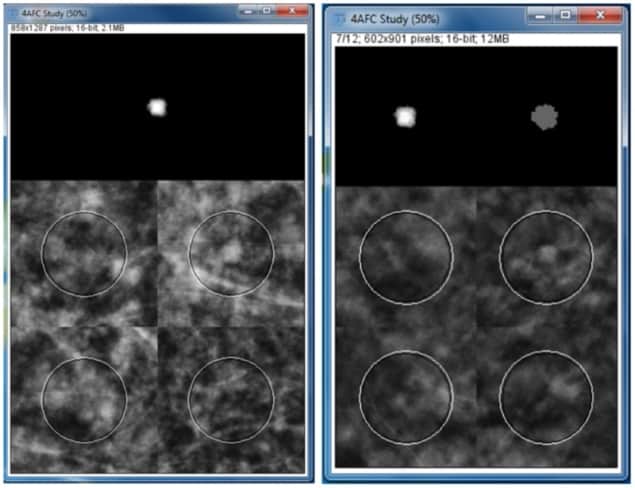
To assess lesion detectability, they performed a 4-alternative forced choice (4-AFC) assessment, in which an observer is shown the target in isolation, plus four image quadrants, one of which contains the embedded target. For the DBT images, a scrollable stack of images mimics DBT viewing conditions. The observers then identify the quadrant that they think contains the target.
The study included 11 specialist (five medical physicists and six experienced clinical readers) and five non-specialist observers. For each observer group, imaging modality and target type, the researchers determined the threshold contrast at which observers made 90.7% correct decisions.
For the 4 mm irregular lesion, the combined threshold contrast for all observers was 6.9% for 2D-mammography and 2.1% for DBT. Similarly, for the 6 mm irregular lesion, the combined threshold contrast was 3.9% for mammography and 0.7% for DBT. DBT also had a lower threshold contrast for the spheres: 2.9% versus 5.3% for mammography, and 0.3% versus 2.2% for mammography, for 4 and 6 mm spheres, respectively. These results demonstrate the superiority of DBT for detecting subtle masses in complex breast structures.
The authors note, however, that a previous study indicated that microcalcifications were detected more reliably in mammography than DBT. They attribute this to the superior ability of 2D systems to detect point-like, high-contrast objects.
Both observer groups found spheres significantly easier to detect than irregular masses. For 2D imaging, the threshold contrast for 4 mm spheres was 1.3 times lower than for 4 mm masses. With 6 mm spheres, differences in contrast threshold were much lower for both mammography (×2) and DBT (×2.7) compared with irregular targets of similar size. The only exception was for 4 mm objects and DBT, where irregular masses were easier to detect.
This difference in threshold contrast between spheres and mass lesions is an important finding as it indicates that studies using only spherical targets may produce over-optimistic detection thresholds.
Are specialists required?
The researchers compared the detection performance of specialist and non-specialist observers, and found that they were generally comparable, with each group marginally outperforming the other in particular tasks.
“We wanted to establish if there were differences in the performance of different types of observers as it is often difficult to find sufficient clinical experts in the types of image assessment trials that we run,” Elangovan noted. “If the performance of non-specialist observers is comparable to specialists then we can conduct such studies at a much faster rate, or even crowd-source the studies to get better statistics.”
Non-specialists required longer reading times than specialists for 4 mm targets, but both had similar reading times for 6 mm targets. The non-specialists’ performance improved after they had seen more data, possibly indicating that increasing familiarity with the task led to faster decision speeds. This supports the use of non-specialists (with training) to supplement the typically limited pool of specialist observers for some tasks.
The researchers concluded that their study quantified the extent of DBT’s superiority over 2D-mammography for detecting masses, as demonstrated by two to eight times lower contrast thresholds. “The results feed into our aim of optimizing how best to use X-ray imaging technology for breast cancer screening and, in particular, how tomosynthesis might be used routinely,” said Elangovan.
The team is now investigating the use of model observers as an alternative to human observers. “This will enable us to run evaluations and comparison studies using a fully simulated approach without time-consuming human observer studies,” Elangovan explained. “We are also studying how differences in the design of DBT systems affects cancer detection and how that in turn will affect the clinical outcomes of screening.”



