A wearable cardiac ultrasound imaging system that can even function during a workout has been developed by researchers from the University of California San Diego. The team hopes that the postage-stamp-sized sensor, which can assess both the heart’s function and structure, will make long-term cardiac scanning accessible to a large population.
According to the British Heart Foundation, in the UK alone, 7.6 million live with a heart or circulatory disease and some 460 people die each day from the same. While cardiac diseases are the leading cause of death among senior citizens, they are also becoming increasingly common among the young.
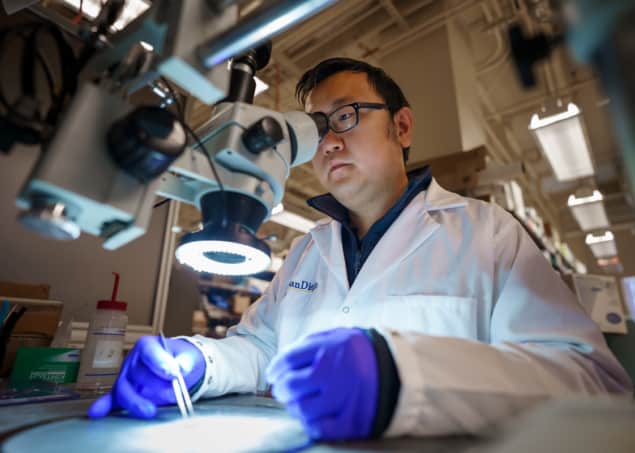
“The heart undergoes all kinds of different pathologies,” explains co-first author and materials scientist Hongjie Hu. “Whether it be that a strong but normal contraction of heart chambers leads to the fluctuations of volumes, or that a cardiac morphological problem has occurred as an emergency, real-time image monitoring on the heart tells the whole picture in vivid detail.”
The problem with cardiac imaging is that echocardiograms typically require highly trained technicians and bulky scanning machinery, whereas CT and PET scans can be uncomfortable for some and come with the added factor of exposing patients to radiation.
Furthermore, many issues with heart function are intermittent, or only become apparent when the body is in motion, the researchers note. Large, fixed pieces of equipment are ill-suited for long-term monitoring, and certainly cannot image moving patients.
In contrast, says project lead and nanoengineer Sheng Xu, the new sensor can be worn for 24 hours in one go, enabling “anybody to use ultrasound imaging on the go”.
Central to Xu and colleague’s system is a wearable, stretchy and adherent patch – 1.9 × 2.2 cm in size, just under a millimetre in thickness and as soft as skin – that emits and receives ultrasound waves. The patch images the structure of the heart in real time and with high spatial and temporal resolution.
Furthermore, artificial intelligence algorithms built into the device allow it to determine how much blood the heart is actually pumping – a vital measurement, as failure to pump enough blood is often at the root of many cardiovascular diseases.
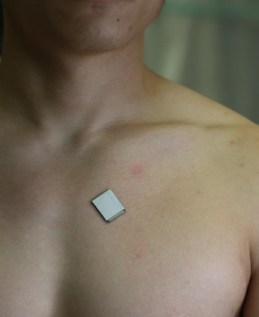
The design of the patch makes it ideal for use on bodies in motion. As co-author and nanoengineer Xiaoxiang Gao notes, it can be attached to the chest with minimal constraint to the subject’s movement, even providing a continuous reading of cardiac activities before, during and after exercise. At present, the patch needs to be connected to a computer via cables, but the researchers say they have developed a wireless circuit to remove this limitation.
“The increasing risk of heart diseases calls for more advanced and inclusive monitoring procedures,” says Xu. “By providing patients and doctors with more thorough details, continuous and real-time cardiac image monitoring is poised to fundamentally optimize and reshape the paradigm of cardiac diagnoses.”
Cardiovascular imaging expert Alastair Moss of the University of Leicester, who was not involved in the present study, says that the system has the ability to “transform” the way doctors monitor and treat heart disease among high-risk patients. “High-quality imaging can help save lives for people with heart disease,” he says. “It is astonishing to think that we will be able to take echocardiography outside of traditional healthcare settings and place it directly in the hands of patients.”
Ultrasound sticker provides continuous imaging of internal organs
Steffen Petersen – a cardiologist at Queen Mary University of London, who was also not involved in this study – agrees, lauding in particular the patch’s ability to provide continuous data feeds during daily activities. He adds: “The potential for such technology in cardiology is huge and assessing cardiac structure and function in such a way will lead to further inventions and clinical indications.”
With their initial study complete, Xu and colleagues are looking to improve the sensor design, miniaturize its power system, and generalize the deep-learning model so it can be used by a larger population of patients. They will also be moving to commercialize the technology – via their start-up Softsonics – over the coming years, with the expectation that a single unit will likely cost around $80 (£66).
The study is described in Nature.