A new generation of MR-guided radiotherapy (MRgRT) systems – capable of visualizing the tumour target during treatment and adapting radiation dose in real-time – is set to transform workflows in the radiation oncology clinic, reducing treatment times, delivering resource efficiencies and improving patient outcomes in the process.
At the biological level, the drivers for MRgRT are also compelling. Tumour shape and position relative to healthy tissue evolve over the course of treatment and can even change during an individual treatment session. The ability of MRgRT to detect those changes and adapt therapy accordingly – in effect, helping clinicians to “see what they treat” in real-time – means that radiation oncology teams are now able to improve the precision of radiation delivery, more effectively treating the tumour while sparing healthy tissue.
Put simply, MRgRT opens the door to personalized medicine tailored to the unique requirements of each patient – for example, adapting radiation delivery to treat tumours that respond rapidly to treatment as well as those that prove unresponsive to standard doses of radiation. That ability to capture the tumour and its environment “on the fly” will, in turn, make it possible to increase the radiation dose to diseased tissue without damaging adjacent organs at risk and other critical structures.
QA best practice
It’s still relatively early days for MRgRT, however, and what constitutes clinical best practice is very much work in progress – not least in terms of defining a rigorous and standardized approach to MRgRT system installation, acceptance, commissioning and ongoing quality assurance (QA).
At the American Association of Physicists in Medicine (AAPM) Annual Meeting in San Antonio, Texas, this week, Modus QA, a Canadian supplier of QA solutions for radiation oncology, will put those MRgRT QA procedures front and centre when it unveils a raft of new features for QUASAR MRI4D, its MR-safe, programmable 4D phantom.
Key areas of emphasis for this latest version of the MRI4D motion phantom include support for QA of MR-linac motion-tracking algorithms and beam latency measurements. Further QA innovation is also in the works for the tracking of complex, deformable motion associated with tumour volumes.
Ultimately, the goal for Modus is to provide the QA tools needed to support radiotherapy OEMs and their early-adopting customers with the clinical roll-out of MRgRT systems. Bringing breakthrough techniques into the clinic requires reliable, end-to-end QA – and in the case of adaptive MRgRT that means MRI-compatible 4D phantoms that make it possible to test the ability of novel MR imaging sequences to track a wide range of tumour motion in the patient (for example, when the patient breathes or when there’s peristaltic motion through the digestive tract).
QA should be simple and quick. It shouldn’t be something that takes our customers a long time.
Enzo Barberi, director of MR product development at Modus QA
The QUASAR MRI4D is designed to do just that on the ViewRay MRIdian and Elekta Unity MR-linacs (as well as other MRI systems such as the Philips Ingenia for MR simulation QA). Thanks to the compact design, users can place the MR-safe 4D phantom in the bore of the magnet to acquire images on low- and high-field strength MRI systems with no induced artefacts or RF noise. Interchangeable inserts are also available for a range of radiotherapy QA procedures spanning imaging, treatment planning, targeting, dosimetry and delivery.
“We spent a lot of time ensuring the simplicity of the set-up for the MRI4D with respect to the MRgRT workflow,” says Enzo Barberi, director of MR product development at Modus. “QA should be simple and quick. It shouldn’t be something that takes our customers a long time, whether they’re MRgRT OEMs or clinical early-adopters.”
Algorithm QA
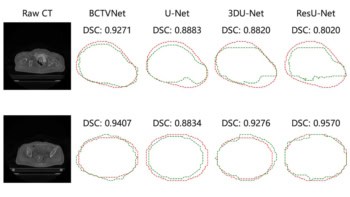
Several of those MRgRT early-adopters are already using the MRI4D for their end-to-end QA, says Barberi, with particular focus on the motion-tracking algorithms used to “gate” the MR-linac’s treatment beam – i.e. rapidly switching the treatment beam on/off as the tumour moves in and out of the radiation field as a result of the patient’s breathing.
To enable these tests, the motion phantom includes a series of rigid targets that can be mounted centrally or offset in an insert to mimic numerous trajectories of a tumour in the body, including those seen during breathing. The insert can move in a linear fashion in and out of the phantom or can combine linear motion with an offset and twist of the target to follow a complex 3D path along the x, y and z directions.
“What we’ve seen in some cases is that this complex motion can confound the MRI tracking algorithms very easily,” says Barberi. “As a result, OEMs and early-adopters are using the motion phantom in the optimization, validation and commissioning of their motion-tracking algorithms.”
Barberi also highlights a work-in-progress R&D initiative to develop a deformable insert for the MRI4D – mirroring the complexity and 4D deformation that tumours are subjected to as a result of motion in the body. “We’re collaborating with STARLIT partners Utrecht University Medical Centre [in the Netherlands] and Elekta Canada to evaluate our tools that allow users, for example, to optimize image-tracking algorithms to follow deformable structures,” says Barberi. “This could be a huge benefit in future with the advent of real-time beam-tracking of the tumour.”
That focus on complex motion and deformation will also be invaluable for OEMs and their customers as they work together on the next generation of tracking algorithms to support faster MR imaging sequences and higher resolutions. “Watch this space,” adds Barberi. “We’ll have one of our proof-of-concept deformable prototypes at our AAPM exhibition booth this week.”
Meanwhile, other MRI-linac sites are using the MRI4D phantom in combination with dosimetry inserts to calculate and measure the dose that is administered to a moving target, ensuring that the treatment beam is actually hitting this moving target and not surrounding healthy tissue. Modus currently offers ion-chamber holders, says Barberi, with a film-cassette holder on the verge of being released.
Minimizing latency
Another new feature of the MRI4D relates to the gating of the MR-linac treatment beams to minimize the effects of patient motion – chiefly from the breathing cycle. With this in mind, the phantom can now provide accurate determination of beam-on and beam-off latency – a feature that will ultimately help to optimize MRgRT gating windows and minimize dosimetric errors.
“The lower the latency the better the job we’re doing in terms of maximizing dose to the target volume and minimizing dose to healthy tissue,” explains Barberi. “We’re not there yet, but down the road – maybe 5–10 years from now – there will be treatment functionality we don’t need – like gating, like breath-hold, possibly even patient immobilization. There are exciting, game-changing innovations taking shape in terms of fast onboard imaging, motion correction and real-time adaptive beam therapy.”
Modus QA is part of the ViewRay partner programme and the Elekta/Philips STARLIT (System Technologies for Adaptive Real-time MR image-guided Therapies) consortium. The aim of these initiatives is to provide next-generation enabling QA and dosimetry capabilities for MRgRT.
Modus QA will be exhibiting on booth 516 at the American Association of Physicists in Medicine Annual Meeting (San Antonio, TX) on 14–17 July.