Advances in radiation therapy have revolutionized the treatment of cancer, but the efficacy of treatment can vary significantly among patients. Recent developments in imaging techniques have enabled clinicians to monitor changes in tumour structure to assess response to radiation therapy.
While structural changes can take weeks to develop, the tumour microenvironment can be a strong indicator of treatment efficacy. Tumours with low oxygenation – hypoxic tumours – are more resistant to radiation therapy. As such, monitoring tumour oxygenation levels in real time could enable personalized treatment delivery, thereby improving treatment efficacy. With this aim, a team at the University of Michigan is investigating the use of photoacoustic (PA) imaging to map tumour oxygen levels.
To obtain PA images, laser pulses are delivered to the tissue of interest. The light is partially absorbed, with the level of absorption dependent upon the laser wavelength and the absorption coefficient of the targeted materials at that wavelength. This absorption of light leads to thermoelastic expansion in the tissue and subsequent emission of ultrasound, which is detected with an ultrasound array transducer and analysed to construct a PA image.
By using multiple incident wavelengths, first author Janggun Jo, senior author Raoul Kopelman and their team have developed a PA functional imaging technology for chemical imaging of tumour microenvironment parameters, such as pH, and potassium or oxygen levels in tissue. They report their findings in ACS Nano.
The researchers combined PA imaging with tumour-targeted chemical construct nanoelements (TTCCNE) that act as PA contrast to visualize the oxygen distribution within the tumour. They created the nanoelements by conjugating the phosphorescence indicator Oxyphor G2 to polyacrylamide (PAA) nanoparticles that have a long phosphorescence lifetime (254–281 µs). Utilizing two laser pulses – the pump and probe beams – the exponential decay of the phosphorescence can be measured. This decay rate strongly correlates to oxygenation levels in the tumour microenvironment.
Photoacoustic lifetime imaging of tumour oxygenation
The researchers developed their photoacoustic lifetime (PALT) imaging technique with the aim of predicting tumour response to radiation therapy.

To assess the technique in vivo, they implanted patient-derived xenografts of triple negative breast cancer, the most aggressive form of breast cancer, within the mammary fat pads of mice. Once the tumour had grown, they injected G2–PAA nanoparticles through the animal’s tail vein, which then accumulated in the tumour.
The team delivered a 630 nm pump beam to the tumour, acting as an excitation source, and used a 920 nm probe beam to monitor the excited state decay, enabling the creation of PALT images of tumour oxygenation. While blood oxygenation only provides an indirect assessment of tissue oxygenation, PALT-based oxygen imaging provides a direct assessment of oxygen levels in tissue.
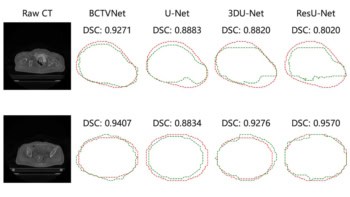
PALT images predict tumour response
Next, the researchers treated the mice with radiation therapy, delivering a total dose of 6 Gy to the tumour at a dose-rate of 1.5 Gy/min. Upon completion of treatment, they harvested the tumours and performed histological staining to determine the distribution of DNA damage.
To investigate whether the method can predict tumour response, the researchers compared the DNA damage with the PALT images obtained prior to treatment delivery. They identified excellent spatial correlation between the pre-treatment tumour oxygen concentration determined using PALT and the radiation-induced DNA damage indicated via histological staining.

Real-time monitoring of brain tissue oxygenation could personalize radiotherapy
At an increased oxygen concentration, the radiosensitivity of cells increases rapidly compared with areas with reduced oxygenation. As spatially resolved PALT images of tumour oxygenation can identify a diverse distribution of hypoxic areas, Jo claims that “PA imaging of tumour oxygenation powered by TTCCNE is capable of predicting tumour responses to radiation therapy, thus enabling personalized treatment decisions”.
The team believes that PA imaging could be generalized further, to monitor the acidity and potassium levels of the tumour, for example. “Using the proper TTCCNE, PA chemical imaging could predict the efficacy of chemotherapy (or of specific drugs), as well as of immunotherapy treatment, for the given patient’s tumour, and thus guide the choice among those three therapies versus surgery,” says Jo.