The Society of Nuclear Medicine and Molecular Imaging (SNMMI) held its Annual Meeting last week. Billed as the “Virtual Edition” and run over an interactive virtual platform, the event included live education sessions, scientific presentations, a virtual exhibit hall and several networking events. Here are some highlights from the research presented at this year’s event.
Total-body dynamic PET successfully detects metastatic cancer
Researchers from the University of California-Davis shared results from the first study using uEXPLORER to conduct total-body dynamic PET scans of cancer patients. Developed and validated at UC-Davis, uEXPLORER is the first total-body (194 cm axial field-of-view), high-sensitivity PET/CT scanner being used commercially. A total-body dynamic PET/CT scan of a patient with metastatic cancer generated high-quality diagnostic images that identified multiple metastases
Dynamic 18F-FDG PET with tracer kinetic modelling has the potential to better detect lesions and assess cancer response to therapy, according to the researchers. Unlike conventional PET scanners with limited axial field-of-view (15–30 cm), the uEXPLORER is capable of simultaneous dynamic imaging of widely separated lesions.
“The focus of our study was to test the capability of uEXPLORER for kinetic modelling and parametric imaging of cancer,” explained UC Davis’ Guobao Wang. “Different kinetic parameters can be used in combination to understand the behaviour of both tumour metastases and organs-of-interest such as the spleen and bone marrow. Thus, both tumour response and therapy side-effects can be assessed using the same scan.”
For the study, a patient with metastatic renal cell carcinoma was injected with the radiotracer 18F-FDG and scanned on the total-body scanner. The researchers calculated static PET standardized uptake values (SUVs) and performed kinetic modelling for regional quantification in 16 regions-of-interest, including major organs and six identified metastases. They calculated the glucose influx rate and used additional kinetic modelling to generate parametric images of the kinetic parameters. The kinetic data were then used to explore tumour detection and characterization. They note that parametric images of the FDG influx rate improved tumour contrast over SUV in general and led to improved lesion detection in the renal cortex, which has been historically challenging.
“Total-body dynamic imaging and kinetic modelling enabled by total-body PET have the potential to change nuclear medicine into a multi-parametric imaging method, where many different aspects of tissue behaviour can be assessed in the same clinical setting – much like the information gained from different sequences in an MRI scan,” said Ramsey Badawi, co-director of the EXPLORER Molecular Imaging Center.
Novel PET radiotracer images malignant brain tumours
A first-in-human study has demonstrated the safety and favourable pharmacokinetic and dosimetry profile of 64Cu-EB-RGD – a new, relatively long-lived PET tracer – in patients with glioblastomas. The radiotracer delivered high-contrast diagnostic imaging in patients, visualizing tumours that express low or moderate levels of αvβ3 integrin with high sensitivity.
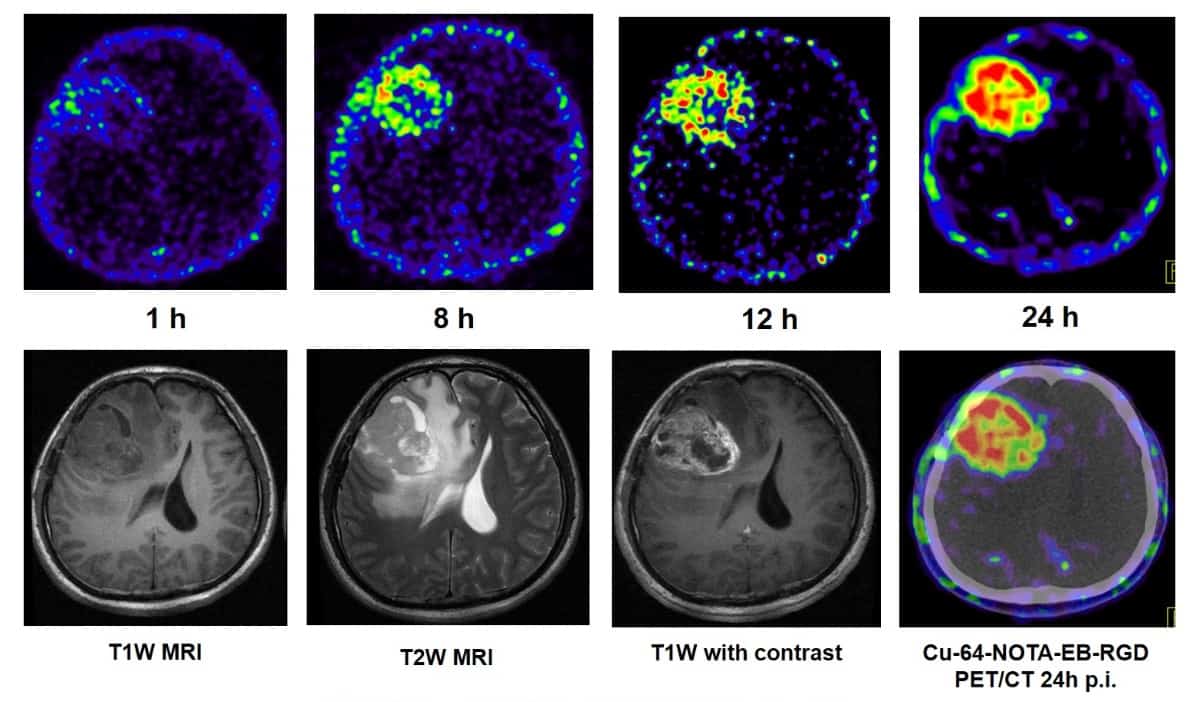
The study included three healthy volunteers and two patients with recurrent glioblastoma who underwent whole-body 64Cu-EB-RGD PET/CT. The new radiotracer has unique qualities, explained Jingjing Zhang, from Peking Union Medical College Hospital. The peptide sequence Arg-Gly-Asp (RGD) specifically targets the cell surface receptor αvβ3 integrin, which is overexpressed in glioblastomas. To slow clearance, Evans Blue dye, which reversibly binds to circulating albumin, is bound to RGD, significantly enhancing target accumulation and retention. The addition of the 64Cu label provides persistent, high-contrast diagnostic images in glioblastoma patients.
The researchers calculated tumour-to-background ratios for target tumour lesions and normal brain tissue in seven sets of brain PET and PET/CT scans obtained over two consecutive days. They also collected safety data (such as vital signs and physical exams, for example) for each participant, one and seven days after the scans.
64Cu-EB-RGD was well-tolerated, with no adverse effects seen immediately or up to one week after administration. The mean effective dose of 64Cu-EB-RGD was similar to that of an 18F-FDG scan. Injection of 64Cu-EB-RGD into patients with recurrent glioblastoma generated high accumulation at the tumour, with continuously increased tumour-to-background contrast over time.
As well as providing a future diagnostic tool, the researchers noted that 64Cu-EBRGD could also be a breakthrough targeted radiotherapy for glioblastoma patients.
“64Cu-labelled EB-RGD represents a viable model compound for therapeutic applications, since 177Lu, 90Y or 225Ac can be substituted for 64Cu,” explained Deling Li of Beijing Tiantan Hospital. “We are currently studying the 177Lu homologue to treat glioblastoma and other αvβ3 integrin expressing cancers, including non-small cell lung, melanoma, renal and bone, and hope to build on the current wave of radiotherapies like 177Lu-DOTATATE.”
PET/MRI approach identifies chronic pain locations
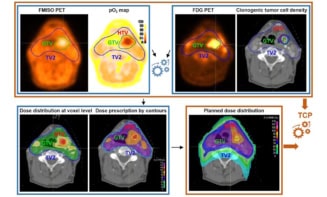
A molecular imaging approach that combines 18F-FDG PET and MRI can precisely identify the location of pain generators in chronic pain sufferers, according to a study from Stanford University School of Medicine. The imaging data led to new management plans for 62% of the study’s participants.
18F-FDG PET has the ability to accurately evaluate increased glucose metabolism that arises from acute or chronic pain generators, such as hypermetabolic inflamed tissues. The researchers sought to develop a clinical 18F-FDG PET/MRI method to accurately localize sites of increased inflammation related to sources of pain.
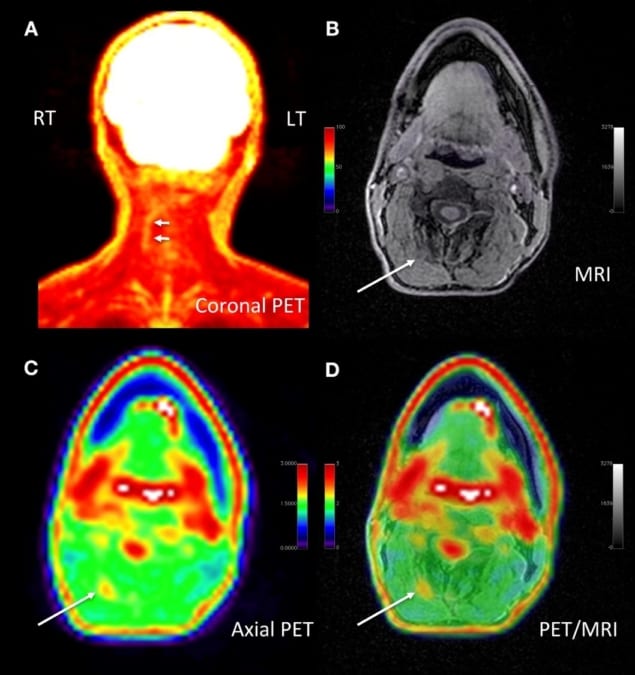
The team imaged 65 patients with chronic pain, from the head to the feet, using the 18F-FDG PET/MRI protocol. Principal investigator Sandip Biswal and colleagues used image analysis software to measure maximum standardized uptake values and target-to-background ratios. They identified locations of increased 18F-FDG uptake and compared these to known locations of pain, finding increased uptake in muscle and nerves at the site of pain in 58 patients.
These imaging findings resulted in 36 significant modifications in management plans, such as the recommendation of new invasive procedures, and 16 mild modifications, such as ordering an additional diagnostic test.
The researchers recommend that a study of a large cohort of patients is conducted to validate their findings. “The results of this study show that better outcomes are possible for those suffering from chronic pain,” said Biswal. “This clinical molecular imaging approach is addressing a tremendous unmet clinical need. I am hopeful that this work will lay the groundwork for the birth of a new subspeciality in nuclear medicine and radiology.”
Targeted radionuclide therapy enhances immunotherapy response
Immunotherapy has had limited success in the treatment of prostate cancer, due to a significantly immunosuppressive tumour microenvironment. Now, a preclinical study conducted at the University of Wisconsin-Madison has shown that targeted radionuclide therapy creates a favourable tumour microenvironment in prostate cancer, which improves the effectiveness of immunotherapies.
“Understanding this treatment dynamic, our goal was to demonstrate that systemically delivered targeted radionuclide therapy provides beneficial immunomodulatory effects that may enhance the response of prostate cancer to immunotherapies,” said Reinier Hernandez.
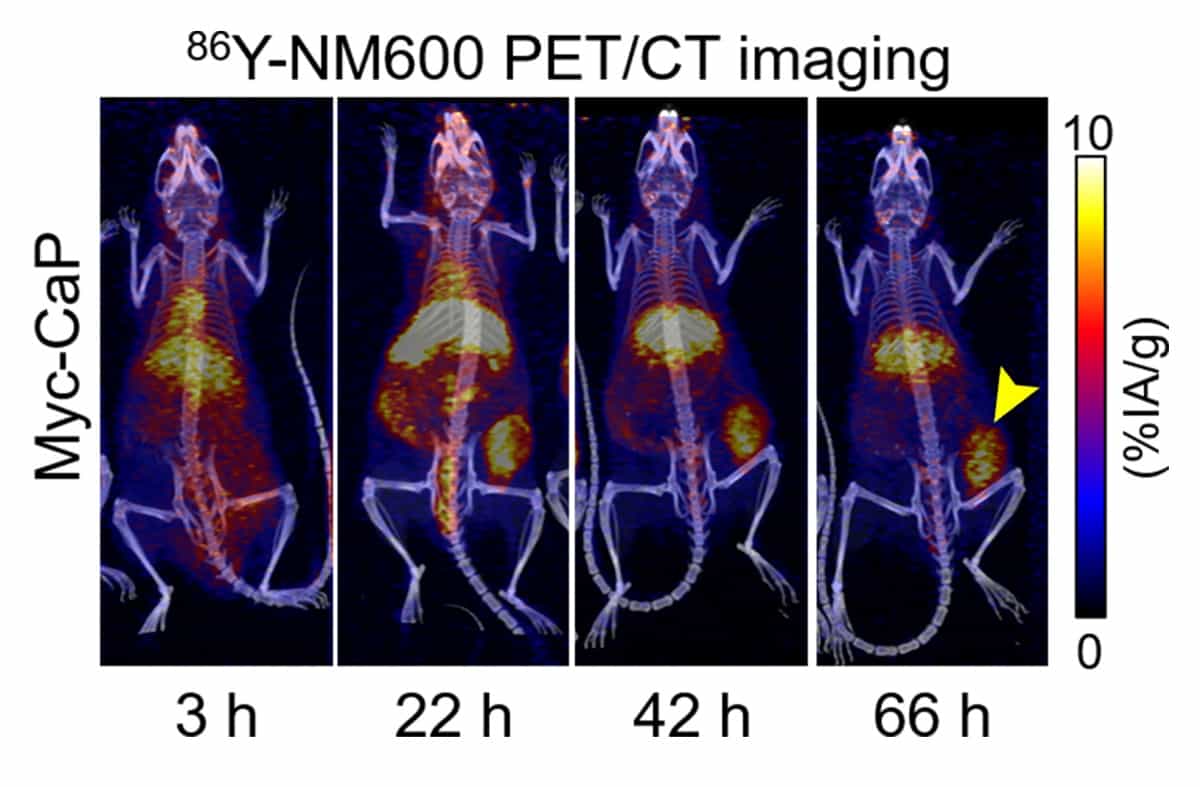
The researchers administered the imaging agent 86Y-NM600 to mice with prostate tumours and performed PET/CT scans 3, 24, 48 and 72 hr after injection. Analysing radiotracer uptake in tumours and in healthy tissues allowed them to estimate the dosimetry for targeted radionuclide therapy using 90Y-NM600. They then gave groups of mice either a high or low dose of 90Y-NM600, and monitored tumour growth and survival for 60 days.
PET/CT data revealed that 90Y-NM600 immunomodulates the prostate tumour microenvironment by modifying tumour-infiltrating lymphocyte populations, upregulating checkpoint molecules and promoting the release of pro-inflammatory cytokines. The team found that 90Y-NM600’s pro-inflammatory effects on the tumour microenvironment were elicited at relatively low radiation doses without incurring systemic toxicity.
“Our results provide a rationale for combining targeted radionuclide therapy with immunotherapies, which, so far, have proven ineffective in prostate cancer. Improving immunotherapy in prostate cancer could bring about a potentially curative treatment alternative for advanced-stage patients,” said Hernandez.
The researchers noted that the study also presents a paradigm change in targeted radionuclide therapy, where the maximum tolerable dose may not always be the most beneficial to patients. “A key finding of our work is that immunomodulation is best achieved with a relatively low radiation dose to the tumour which does not affect the normal immune system,” Hernandez explained.