The coronavirus responsible for the current COVID-19 pandemic is transmitted through respiratory droplets and aerosols emitted when people cough, sneeze, talk and breathe. Face masks reduce transmission by trapping many of these infectious particles at their source, but questions remain over which mask types and materials are most effective. A team of researchers at Cambridge University in the UK has now developed non-contact, wearable, portable sensors that measure the amount of moisture that leaks through a face mask during normal breathing, rapid breathing and coughing. The new devices are based on transparent, micron-sized electronic fibres, and the researchers report that they significantly outperform comparable commercial sensors.
One-step printing process
Sensors made from small conducting fibres are especially useful for measuring volumes of fluids and gases. However, such fibres are hard to print and incorporate into electronic devices, while manufacturing them at scale poses additional difficulties. One challenge is that the high aspect ratio of these mechanically flexible and transparent small-diameter conducting fibres makes them hard to manipulate individually. To handle these fragile fibres, therefore, transparent nano- and micro-fibre-based devices are generally mounted on a substrate. The downside is that such substrates mask the very optomechanical properties that the sensor is designed to exploit, and they also drastically reduce the surface area-to-volume ratio of the fibre array. In addition, circuits with good fibre-to-fibre conductivity often require multiple procedures or post-fibre synthesis treatments to make.
To overcome these problems, team leader Yan Yan Shery Huang and colleagues developed a quick, one-step fibre manufacturing process that they call inflight fibre printing (iFP). The process begins with a mixture of silver or a biocompatible conducting polymer known as PEDOT:PSS. During printing, the silver/PEDOT:PSS solution is heated to ensure that it rapidly solidifies, and a core-shell nozzle is used to coat it with a thin (10-20 nm) layer of polyethylene oxide. The result is a highly pure conducting-core fibre structure that is encased in a protective polymer sheath and can be connected to copper contact pads with minimized contact resistance. Notably, the iFP technique creates and bonds thin, conducting fibre arrays directly, without any need for post-processing.
Free-standing and permeable to moisture flow
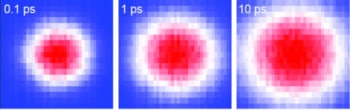
In addition to their good optoelectrical characteristics, the free-standing nature of the team’s iFP PEDOT:PSS fibre arrays makes them permeable to moisture. By measuring how the resistance of end-to-end fibres evolves in response to changes in humidity, Huang and colleagues were able to organize the fibre arrays in a way that optimizes their sensitivity to these changes. The result is a system in which the resistance of the iFP fibres increases linearly as relative humidity rises from 55 to 90% at room temperature. The researchers also report that their iFP fibres responded faster than a commercial humidity sensor when sprayed with a mist of water.
To test their iFP fibre arrays, the researchers fabricated two types of respiratory moisture sensor. In the first, they printed a single layer of PEDOT:PSS onto a 3D-printed plastic frame to create a sensor that attaches to the exterior of a disposable mask. The team found that the resistance of the fibre arrays in this wearable, non-contact and non-invasive respiration-rate monitoring device returned to its baseline level less than three seconds after normal breathing. A commercial sensor, in contrast, takes roughly 10 seconds. What is more, unlike commercial sensors, the fibre-array sensor proved adept at detecting rapid breathing patterns (roughly 1.2 seconds per breath cycle) that can indicate shortness of breath.
COVID-19: how physics is helping the fight against the pandemic
The second type of sensor consisted of PEDOT:PSS fibre arrays as front and back layers, with a sound-detecting suspended piezoelectric polymer nanofibre layer sandwiched in between. Since the entire sensor is transparent and permeable to air, the researchers say that it could be attached to a phone camera and used to collect multiple types of information – such as image, sound and local spatial variations in breath humidity – at the same time.
Detecting the flow of respiratory moisture
In a final series of experiments, Huang and colleagues configured their system to detect respiratory moisture that flows through a mask when the wearer breathes and coughs. In surgical masks, they found that most moisture leakage occurs at the front – implying that such masks redirect some exhaled breath out around the nose area and through the front of the mask. N95 masks tended to leak from the top and sides while FFP2-grade masks – which are designed to filter out at least 94% of airborne particles – were found to be more effective at reducing the flow of breath through the front of the mask. Both types of mask, however, weakened the flow of exhaled breath when worn correctly. The team also found that when a mask-wearing person coughs, the resistance of the fibres increases much more steeply than when the person lets out a long breath – confirming that the strength of the airflow during coughing is higher than when exhaling normally.
According to the researchers, who report their work in Science Advances, portable sensors like these could find use in mobile-health diagnostics and assessments, where their low cost (at 50p for the single-layer sensor and around £2 for the tri-layer device) makes them particularly attractive. The fibres themselves may also have biological applications beyond respiratory sensing. Because the fibres can be made with diameters below the typical size of a cell (a few microns), the researchers say they could be used to guide the movement of cells and detect this dynamic process as electrical signals.