The latest novel coronavirus, SARS-CoV-2, has reached pandemic status. While health workers and governments do their part, scientists are trying to understand the virus and develop vaccines and treatments. Jon Cartwright looks at how physics plays an important role in the fight

It probably originated in one of the several species of horseshoe bat found throughout east and south-east Asia. Possibly, a pig or another animal ate the bat’s droppings off a piece of fruit, before being sold at a wet market in Wuhan, China, and subsequently infecting one of the stallholders. Or maybe the first transmission to a human occurred elsewhere.
There is a lot we don’t know about the novel coronavirus now called SARS-CoV-2 and its resultant disease, COVID-19. What we do know is that Chinese authorities alerted the World Health Organization (WHO) to the first known cases in Wuhan at the end of last year. Less than a fortnight later, one of those infected people was dead. By the end of January, with more than 10,000 diagnosed cases and 200 fatalities in China alone, and with the virus cropping up far beyond the country’s borders, the WHO declared a global emergency.
As of this article’s publication (19 March), the WHO reports that the virus has spread to 166 countries, areas and territories, with over 205,000 confirmed cases worldwide and the number of deaths exceeding 8500. The status of “pandemic” was officially designated on 11 March and many countries have introduced social distancing, travel restrictions and quarantine methods to try to curb the spread. Festivals, sports events, parades and conferences are being called off due to the front-line support services they require and the concern that large gatherings of people could help spread the virus. The American Physical Society, for example, axed both its annual March meeting in Denver, Colorado, and April meeting in Washington DC.
When it comes to viruses, there is good reason to worry about novelty. Throughout its history, humanity has had to contend with new diseases springing up seemingly out of nowhere, spreading like wildfire and leaving scores of dead in their wake. In ages past, bacterial plagues were often the source of that terror. Since the birth of modern medicine, however, novel viruses have assumed the mantle of doom. Take Spanish flu for example, which killed up to 100 million people a century ago, and then more recently, HIV, which has led to around 32 million deaths to date. It is only a matter of time before another devastating pandemic, and though epidemiologists do not know what type of virus it will be, they do know that it will be different from anything witnessed before.
Whether or not SARS-CoV-2 is the next “big one”, there is something else epidemiologists are grimly aware of: today, disease travels fast. The Black Death that ravaged Europe, as well as parts of Asia and Africa, in the mid-14th century spread at an average of just 1.5 km a day – hardly surprising, since this was before ships could reliably cross oceans and the fastest mode of transport was by horse. Contrast that with the 2015 outbreak of Zika virus in South America, where the daily dispersion was on average 42 km, peaking in the densest-populated parts of Brazil at 634 km. Faced with more populous cities, more mobile people and more international travel, scientists must respond to the threat of viral pandemics faster than ever.
Structural biology has reached the stage where it’s fast enough for almost anything
Fortunately, those scientists now have much more efficient tools at their disposal. Structural biology – the study of the structure and function of biological macromolecules – has come a long way since it was first used as the basis of rational (as opposed to trial-and-error) drug design 30 years ago. Back in the early 1990s, viral structures deposited in the Protein Data Bank – an international repository for structures of biological macromolecules – numbered just a few dozen annually, but by the mid-2010s, there were well over 500 new additions a year. Modern techniques, such as automation and cryo-electron microscopy (cryo-EM), mean that viral structures can be identified almost instantly in many cases. “Structural biology has reached the stage where it’s fast enough for almost anything,” says Alexander Wlodawer, chief of the macromolecular crystallography laboratory at the US National Cancer Institute in Frederick, Maryland.
But is it fast enough to halt a pandemic?
The speed of physics
Physics-based techniques play a huge role in the field of structural biology. The vast majority of biological macromolecule structures are obtained by X-ray crystallography, going back to 1934, when John Desmond Bernal and Dorothy Hodgkin recorded the first X-ray diffraction pattern of a crystallized protein, the digestive enzyme pepsin. Their work stemmed from that of physicists such as Wilhelm Röntgen, who discovered X-rays; Max von Laue, who discovered that X-ray wavelengths are comparable with inter-atomic distances and are therefore diffracted by crystals; and William Henry and William Lawrence Bragg, who showed how to use a diffraction pattern to analyse the corresponding crystal structure. Hodgkin went on to win the 1964 Nobel Prize for Chemistry for her determinations by X-ray techniques of the structures of important biochemical substances.
Single biological molecules also diffract X-rays, but only very weakly. Crystallization, as Bernal and Hodgkin employed for pepsin, is helpful because it results in the repetition of huge numbers of molecules in an ordered, 3D lattice, so that all their tiny signals reinforce one another and become detectable – by photographic plates in the early days and by active pixel detectors today. These signals are not images of the molecules, for there are no materials that can substantially refract, and thereby focus, scattered X-rays. Rather, the signals are merely the sum of the contributions of X-rays diffracted from different parts of the molecule. To pick apart these contributions, structural biologists rely on a mathematical tool – the Fourier transform. The calculated contributions are then equated with possible atomic structures by a lot of careful (and now largely computer-driven) interpretation.
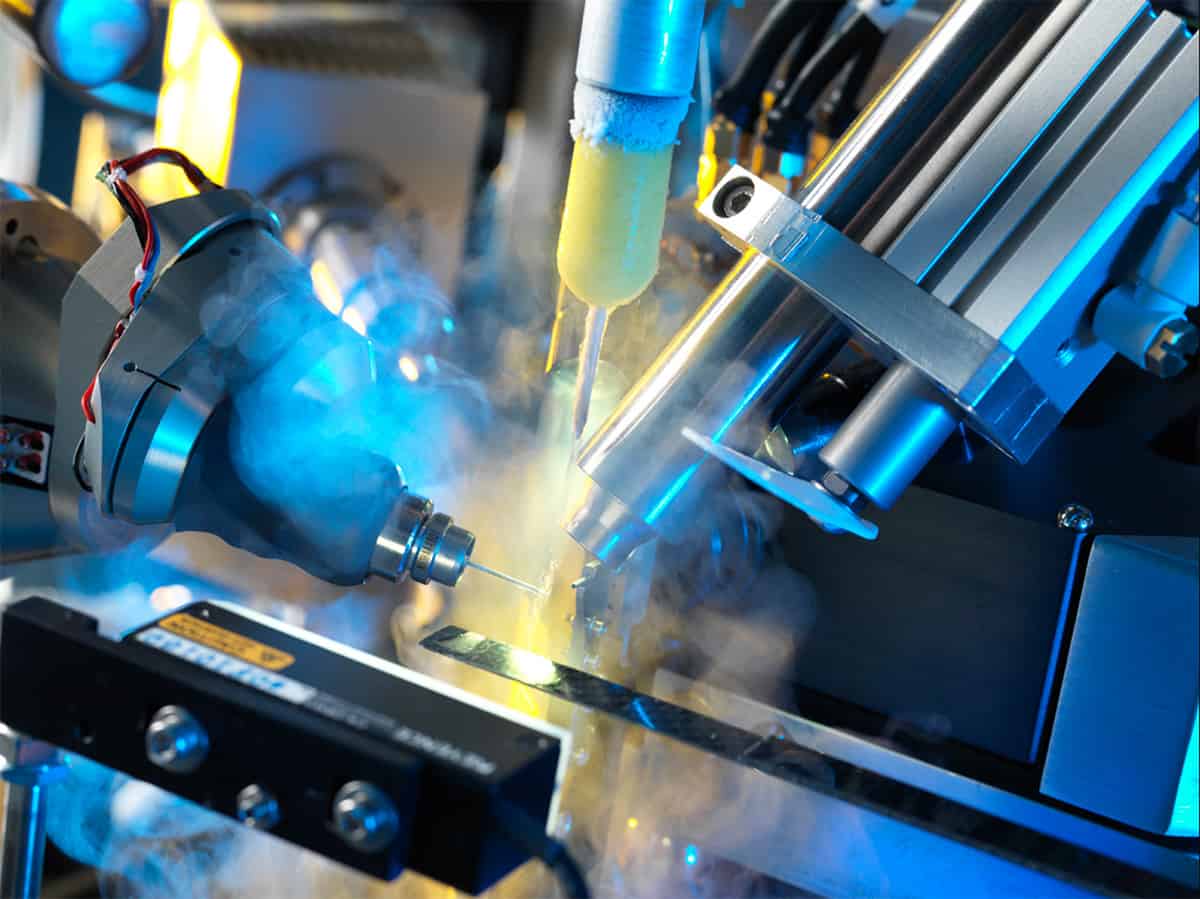
Of course, to obtain the signals in the first place requires X-rays. Nowadays, synchrotron radiation sources – large facilities that accelerate electrons in a continuous ring – are ideal for macromolecular crystallography because they produce high-intensity X-rays with a very narrow spread of wavelengths. At these machines, according to Wlodawer, diffraction datasets that would have taken months with X-rays from traditional rotating anode generators take just seconds to compile.
Technological developments such as these spurred the first forays into rational drug design, in which scientists study the structure and function of molecules in order to work out what drugs might bind to them – and in the case of viruses, prevent them from replicating. Antiviral drugs for HIV were an early success. When HIV protease was identified in 1985 as an essential enzyme – and therefore a potential drug target – in the virus’s life cycle, it took four years for its first crystal structures to be determined, and a further six years for the first licensed drugs to inhibit it. “That’s probably one of the best-documented cases of how quickly rational drug design can go,” says Wlodawer, who contributed to the international effort.
Today, it might have gone faster. The four-year delay in obtaining the structure of HIV protease was primarily due not to the brilliance or quality of X-rays, but to the lack of sizeable crystals of the enzyme. Current synchrotrons and ever newer free-electron lasers – which extract diffraction data from molecular crystals in the few femtoseconds before they are annihilated – employ techniques such as serial crystallography to build up a complete diffraction dataset from numerous partial datasets of crystals that would otherwise be too small. Moreover, both the crystallization and data collection are now automated, so that structural biologists need not even visit a light source themselves: they simply post their proteins to a facility and download the dataset when it is ready.
The analysis of SARS-CoV-2 is a prime example of this type of modern pipeline in action. On 5 February this year, a little over a month after the Chinese authorities disclosed the existence of the new coronavirus, a research team led by Zihe Rao and Haitao Yang at ShanghaiTech University in China uploaded the structure of the virus’s main protease to the Protein Data Bank (DOI: 10.2210/pdb6lu7/pdb), having obtained the dataset using X-ray crystallography at the Shanghai Synchrotron Radiation Facility. “A decade ago, that would have taken a year,” says Wlodawer. “At least.” The structure is already helping pharmaceutical companies to explore potential drugs, such as those used to tackle HIV.
The protein pipeline
Even if molecules refuse to be crystallized, there is still the chance of obtaining structures using cryo-EM, a technique pioneered by Jacques Dubochet of the University of Lausanne in Switzerland, Joachim Frank of Columbia University in New York City, US, and Richard Henderson of the MRC Laboratory of Molecular Biology in Cambridge, UK, for which they shared the 2017 Nobel Prize for Chemistry. In a cryo-EM experiment, a solution containing the biomolecule or complex of interest is applied to a sample holder, or “grid”, as a thin layer. The grid is flash-frozen in liquid ethane to vitrify the sample, which is then imaged by the electron microscope with low doses of electrons to minimize radiation damage. Because single molecules or complexes are imaged directly, there is no need for crystallization.

Thanks to cryo-EM, Daniel Wrapp and Nianshuang Wang of the University of Texas at Austin, US, and colleagues were able to obtain the structure of an outer “spike” protein of SARS-CoV-2 that is believed to enable the new virus to weasel its way into host cells. From harvesting the protein to submitting a paper to the journal Science on 10 February, the entire process took just 12 days (10.1126/science.abb2507). “Without cryo-EM,” says the University of Texas’s Jason McLellan, an author on the paper, “it may not have been possible at all.”
The structure of the external spike is more useful for creating coronavirus vaccines than drugs. If host cells are exposed to virus-like particles that brandish the same external features, while being hollow inside, those cells can still help the body build an immunity but without the risk of being exposed to a dangerous, fully fledged virus. David Stuart – a structural biologist at the University of Oxford in the UK and director of life sciences at the Diamond Light Source, a “third-generation” synchrotron – has used this synthetic trick to create a new vaccine for foot-and-mouth disease. This virus, which is still devastating livestock in large parts of Africa, the Middle East and Asia, is in a family of single-stranded “positive sense” RNA viruses that also includes polio and human rhinovirus – the latter being behind most cases of the common cold. “Only in the past few years have we been able to exploit structural biology to understand immunity to disease,” he says. The knowledge of viral structures can even be used to design synthetic “therapeutic antibodies” to directly attack diseased cells, he adds.
Stuart obtained the structure of the foot-and-mouth virus itself back in 1989 at the (now defunct) Synchrotron Radiation Source in Daresbury, UK. Indeed, it was one of the first viral structures ever deposited in the Protein Data Bank. For that reason, he knows first-hand how much the techniques have progressed. “Getting those first structures, that was a big deal!” Stuart recalls.
Beware the unknowns
It is too early to predict how long it will take to develop drugs or vaccines for SARS-CoV-2. A US biotechnology firm, Moderna Therapeutics, has already begun human trials for a vaccine candidate, but even if it successful, it could still take up to 18 months for it to be available to the public. Borrowing the infamous terminology of the former US defence secretary Donald Rumsfeld, Stephen Cusack – the head of the European Molecular Biology Laboratory (EMBL) in Grenoble, France – puts the virus in a category of formidable “unknown unknowns”, which covers viruses that break out without precedent, such as HIV, Zika and the 2002 coronavirus, SARS-CoV. But Cusack says we should still beware the more familiar “known unknown” pandemic influenza, which has struck three times since the Spanish flu of 1918. Its most recent incarnation in 2009, swine flu, is believed to have infected up to a fifth, and killed up to half a million, of the world’s population – although that, relatively speaking, was not such a bad case. Similar numbers are met every year with seasonal flu – in Cusack’s terminology, the “known known”.
Though he graduated as a physicist, Cusack has spent much of his career studying influenza as a structural biologist, and in particular its polymerase – the enzyme behind the virus’s transcription and replication. Like other viruses, in order to replicate, influenza has to produce a code for its proteins known as messenger RNA (mRNA). This needs to match the mRNA of the healthy host cell that the virus is invading in order to trick the cell to produce more of the virus. Some viruses have their own enzymes to synthesize the matching mRNA from scratch; influenza does not, and instead steals a “cap” from the host-cell mRNA as a primer. Biochemists have known of this influenza “cap snatching” for many years, but in 2014 Cusack’s group used structural-biology techniques to understand its basic mechanism at an atomic level. In their most recent work, yet to be published, the researchers have employed cryo-EM to snapshot different stages of the entire polymerase transcription – in effect creating a molecular movie – in order to uncover weaknesses that can be targeted by drugs. “If you can stop this mechanism from working, you can stop the virus from replicating,” Cusack says.

Physics joins the fight against the coronavirus, philosophical differences of physics and chemistry, escape to an exotic exoplanet
All of which suggests that structural biologists are well-equipped to tackle the next pandemic, be it a known-unknown or unknown-unknown. Whether their techniques are sufficiently advanced to prevent some of the huge death tolls humanity has suffered in the past, however, is still an open question. Those who study complex networks believe they can now predict the rate at which pandemics spread in the modern world (see box below), although these only stress the shortness of the deadlines on which scientists must act. Moreover, finding a drug is only the first step in a long regulatory process involving fabrication, initial toxicology testing and clinical trials.
Even then, there is no guarantee of success. In 2018 Xofluza was the first antiviral drug for influenza approved by regulators in Japan and the US for decades, billed by the press as a “miracle cure” that was able to stop the virus dead in its tracks just 24 hours after a single dose. A year later, the Japanese company that developed it, Shionogi, discovered that, far from being killed off, the virus in patients taking the drug spontaneously mutated into a more resilient form. Working with Shionogi, Cusack and colleagues used structural-biology techniques to show that although the mutated virus bound to the drug less tightly, it was also less fit to replicate, leaving a question mark over the drug’s efficacy. “No-one knows whether the drug will be useless in a year or two,” he says.
And therein lies a lesson. “The virus is always cleverer than you are,” Cusack says. “But we knew that anyway.”
The global village

Back in the 14th century, when the bubonic plague known commonly as the Black Death was advancing through Europe, geographical proximity to an infected town or village was a reliable indicator of how likely a neighbouring settlement’s inhabitants would contract the disease. In today’s globalized world, however, with the ease of long-distance travel, that is no longer true – at least according to the physicist Dirk Brockmann of Humboldt University Berlin in Germany and the physicist-turned-social-scientist Dirk Helbing of ETH Zurich in Switzerland. In 2013, based on an analysis of airports, the pair showed that computer models could better describe the progress of previous epidemics, such as the swine flu of 2009, if they spread through an “effective” distance between points – one that is dependent not on miles or kilometres but the density of traffic flow between them (Science 342 1337).
Although their model – and others like them – could be important for predicting the spread of current viruses and targeting disease-control measures, population flow between cities is not always known to high accuracy. In a preprint posted online in February this year, however, Piet Van Mieghem and colleagues at the Delft University of Technology in the Netherlands showed that it is possible to make short-term predictions about the rate of progression of the latest coronavirus, SARS-CoV-2, from Wuhan to other cities in the Chinese province of Hubei if population interactions between cities are inferred from initial observations of the spread, rather than relying on prior knowledge. Comparing their model with real data, they found that its predictions for infections in Hubei cities three days ahead were within 7.5% of the actual numbers (arXiv:2002.04482). “The coronavirus pandemic has been a good case to demonstrate the power of our method,” says Van Mieghem.