Blood clots in an artery – otherwise referred to as an arterial thrombosis – are potentially fatal, and are a major risk factor leading to strokes and heart attacks. One way to study this problem in the lab is to exploit precise manufacturing techniques like 3D printing, and mimicking the interaction between vessel walls and blood flow is critical to effectively replicating healthy and diseased blood vessels in vitro.
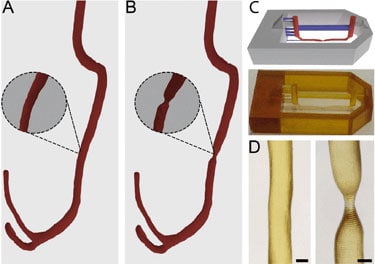
Researchers in the Netherlands have now created a more accurate blood-vessel model that effectively replicates the formation of a blood clot caused by stenosis defects, the narrowing of a blood vessel that can lead to disease (Lab on a Chip 18 1). The researchers, from the University of Twente and Utrecht University, developed a microfluidic blood-vessel model using layered stacks of computed tomography angiography (CTA) data combined with sterolithography, a light-based 3D-printing process.
To create the model, the researchers first 3D printed a negative mould with the precise blood-vessel structure. They then poured a mixture of polydimethylsiloxane (PDMS) and a crosslinking agent mixture into the mould, which was then cured to create the vessel channel. By lining the vessel channel with endothelial cells and perfusing patient blood at normal arterial shear rates, the researchers established the platelet aggregation that forms a blood clot, and they also observed an increase in the backflow downstream of the stenosis defect.
Improvements in geometry
The anatomically accurate blood vessel model developed by these researchers achieves an even distribution of shear stress across the vessel, which makes it much more clinically relevant than typical in vitro models. The key difference is the geometry of the fabricated blood vessel, since most previous microfluidic models have been produced with a square channel where vessel cells can be seeded and perfusion can occur. These square channel walls do not provide an accurate representation of a blood vessel, with differing shear forces being applied to the corners and flat sections of the square vessel.
Results produced from this 3D model can be cross-referenced easily with fluid-flow simulations in silico to instil a systems biology approach to research, and the researchers believe the use of patient CTA data could lead to the development of patient specific blood-vessel models. The resolution and control of the blood vessels produced by the technique also makes it suitable for modelling alternative vascular diseases, including chronic conditions like vascular dementia. Further development of this model could eventually lead to a fully stratified approach to vascular disease research, which in turn would reduce the number of animals used in research studies.