An Italian-led research team has developed a technique that can use augmented reality instead of conventional intraprocedural imaging to guide needle insertion for interventional procedures, according to research published in European Radiology Experimental.
The group, led by first author Marco Solbiati of advanced visualization firm R.A.W., created augmented reality software capable of using a tablet to project 3D models of CT scans directly onto a target. They found that applying this technology to needle insertion — a common first step for the interventional oncology procedure thermal ablation — allowed clinicians to simulate the task well within a 5-mm accuracy threshold (Eur. Radiol. Exp. 10.1186/s41747-018-0054-5).
This proof-of-concept study for the device was the first time that clinicians were able to target focal liver lesions using augmented reality only, wrote Solbiati and colleagues from various institutions in Italy, Israel and the US.
“Indeed, our investigation demonstrates that an augmented reality system can provide accurate guidance for interventional oncology procedures … without the need for further real-time intra-procedure imaging (such as ultrasound or CT), thereby avoiding possible exposure to ionizing radiation and the need for an additional co-registered modality,” they wrote.
Three-step experiment
Highly accurate image guidance is critical for the success of minimally invasive procedures performed in interventional oncology, a growing offshoot of interventional radiology, the authors noted. During surgery, clinicians in this field most commonly refer to a display of MRI or CT scans to guide intricate procedures such as thermal ablation. But this requires them to frequently look back and forth between the patient and the screen as well as mentally reconstruct the 2D scans into 3D images while performing the operation.
“Efforts have recently been made not only to improve the efficacy of ablative devices, but also to increase the accuracy of image-guiding systems,” the authors noted. “Several navigation systems have been developed using augmented reality techniques … [that] allow the operator to see 3D virtual objects superimposed upon the real world and not on a different screen.”
Seeking to improve the precision and efficiency of image guidance for interventional procedures, Solbiati and colleagues developed a new technique that relies on augmented reality instead of conventional radiographic imaging for visualization.
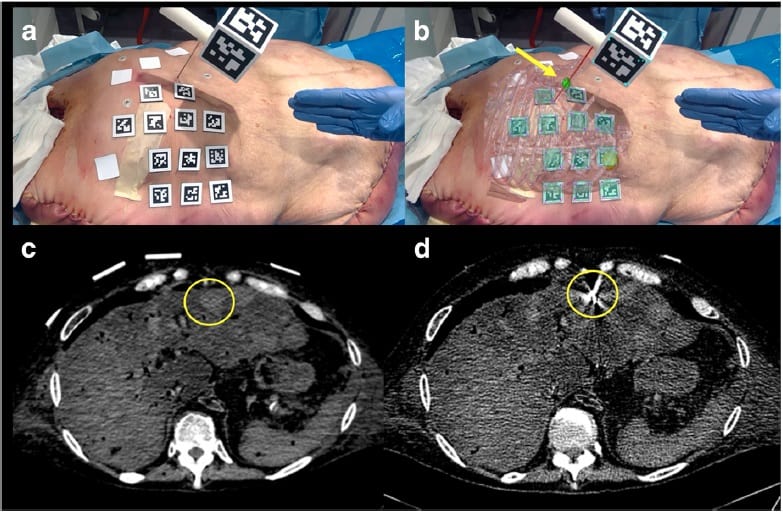
They created their augmented reality software (Endosight, R.A.W.) in a computer program (Unity 2017.1.1, Unity) and designed the software to superimpose 3D images directly onto a target. The augmented reality device includes a customized needle handle and a tablet (Microsoft Surface Pro 4, Microsoft) attached to a tripod that can display 3D images through its camera.
To test the accuracy of the technology, the researchers simulated needle insertion for thermal ablation using the augmented reality device on three different models: a custom-made silicone phantom, a pig and a cadaver with liver metastases.
First, they placed radiopaque skin markers on each of the models, acquired and processed CT scans of the models, and converted the scans into 3D images for the augmented reality software. Then the investigators used the augmented reality device to project these 3D images directly onto the corresponding model. This allowed the clinicians to visualize the targeted area for insertion in relation to relevant internal structures as they manoeuvred the needle.
High targeting accuracy
Overall, the tests for augmented reality guided needle insertion demonstrated extremely high accuracy — within the threshold of 5 mm from the targeted site. The average distance between the geometric centre of the model and the augmented reality images was 2 mm for the phantom, 3.9 mm for the pig model and 2.5 mm for the cadaver. The mean distance was 2.8 mm for the two liver tumours in the cadaver.
For the pig model, the mean amount of time it took to set up the device was 5.3 minutes, and the average time to perform needle insertion was 7.2 minutes. For the cadaver, the average set-up time was 5.8 minutes and the average procedural time was 9.4 minutes.
With the aid of the augmented reality device, clinicians may be able to visualize 3D models of organs and thermal ablation targets superimposed on real patients rather than on a different screen — improving the treatment result, the authors noted.
They are currently working on additional improvements for the prototype augmented reality device, including reducing the number of skin markers required for alignment and using fibre optics to detect needle bending during insertion in real-time.
“The application of augmented reality to interventional procedures might have a relevant impact in further improving the precision of guidance during ablation and holds the potential for a large diffusion in the near future,” they concluded.
- This article was originally published on AuntMinnieEurope.com © 2018 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.