Carbon-ion radiotherapy, a type of charged particle therapy, provides superior dose distribution to intensity-modulated radiation therapy (IMRT) using high-energy X-rays. In Japan, it is being investigated as an alternative to breast conservation surgery for patients with early-stage, localized breast cancer, in a clinical trial that began in April 2013.
Carbon-ion therapy can be delivered in two ways: via passive or scanning irradiation. A new study comparing dose distributions of the two delivery methods revealed that both were appropriate, and that neither method was superior to the other, owing to the characteristics of stage I breast cancer. These findings imply that this treatment can be safely offered to select patients at any type of facility offering carbon-ion radiotherapy (J. Radiat. Res. 10.1093/jrr/rry052).
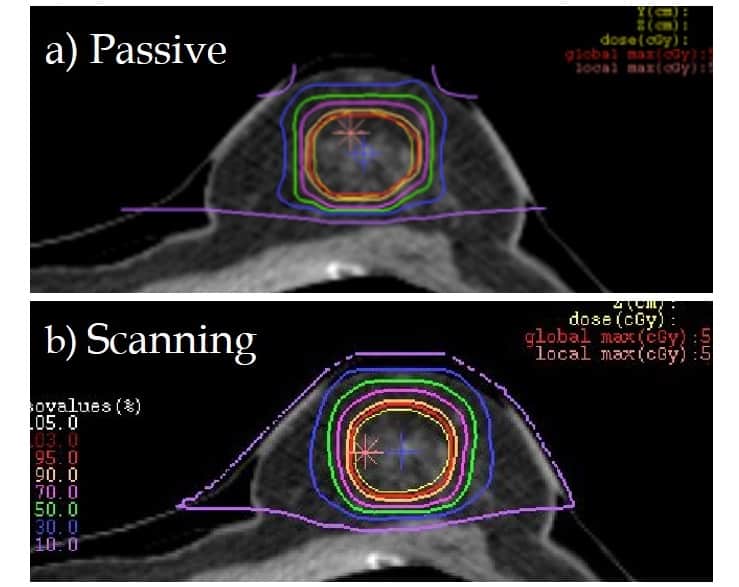
The scanning irradiation method of carbon-ion radiotherapy uses scanning magnets to actively scan a target volume in three dimensions. Because this 3D capability may achieve more flexible dose distribution, it is hypothesized that scanning irradiation may be superior to the passive method of carbon-ion radiotherapy. The passive method uses wobbling magnets, which create a broadened beam that covers the target area in two dimensions.
The patient cohort included 11 women who received passive irradiation carbon-ion radiotherapy in lieu of surgery at the National Institutes of Radiological Sciences (NIRS) Heavy-Ion Medical Accelerator in Chiba. All patients had low-risk disease with a distance of less than 5 mm between the tumour and the skin surface. They received doses of either 48.0, 52.8 or 60.0 Gy, in four fractions.
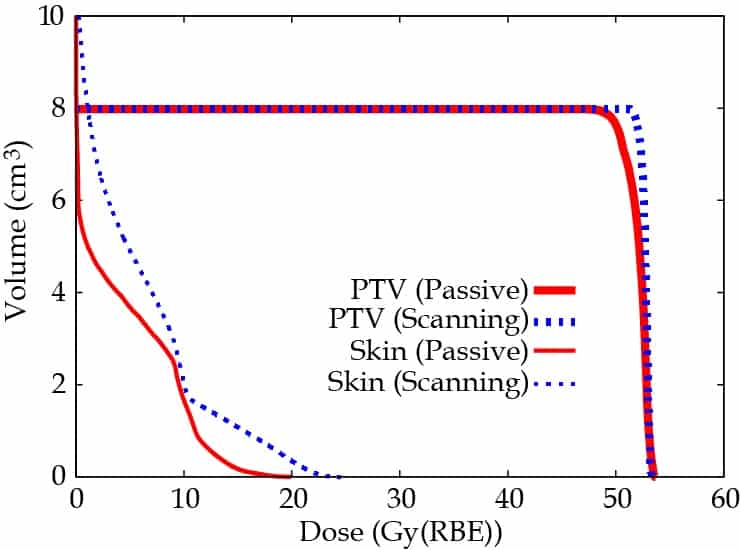
Researchers at NIRS and the Tokyo Women’s Medical University created treatment plans for the scanning irradiation method. They evaluated both plans by examining the dose concentration on the target, assessing the dose delivered to 95% of the planning target volume. The dose delivered to organs-at-risk (OAR) was considered acceptable as long as the skin dose did not reach half of the prescribed dose.
The doses delivered by each method varied among patients, with both plans achieving a high dose for some patients, and other patients having both plans deliver a low dose. However, statistical analysis showed that there was no significant difference in superiority between the two methods. These findings surprised the researchers, according to lead author Hiroaki Matsubara from Tokyo Women’s Medical University.
The researchers attributed the lack of significant difference in part to the shallow locations of the tumours, which enable a low-energy carbon-ion beam to be employed for the treatment. “As a result, the dose distribution quality by the scanning irradiation method deteriorates owing to blurring of the lateral component of the beam, but the quality of the passive method does not change because of the usage of the patient collimator,” the authors wrote. They did caution that findings might change for treatment of women with deeper tumour locations.
Additionally, because skin was the only organ treated as an OAR, the spatial configuration between the target tumour and the OAR was “simple”. And as the shape of the target of breast cancer is simply globular, this treatment does not require a complicated dose distribution.
“It is valuable to know that the scanning irradiation method may not always be superior to the passive method,” the authors concluded, noting that in some cases the passive irradiation method could provide better dose distribution.



