Chemotherapy and radiotherapy are standard treatments used after cancer surgery to destroy any residual tumour cells within the surgical cavity or circulating in the body. Such therapies, however, can be associated with adverse effects. Cold atmospheric plasma could provide an alternative anti-cancer tool and is under investigation as a potential postsurgical treatment.
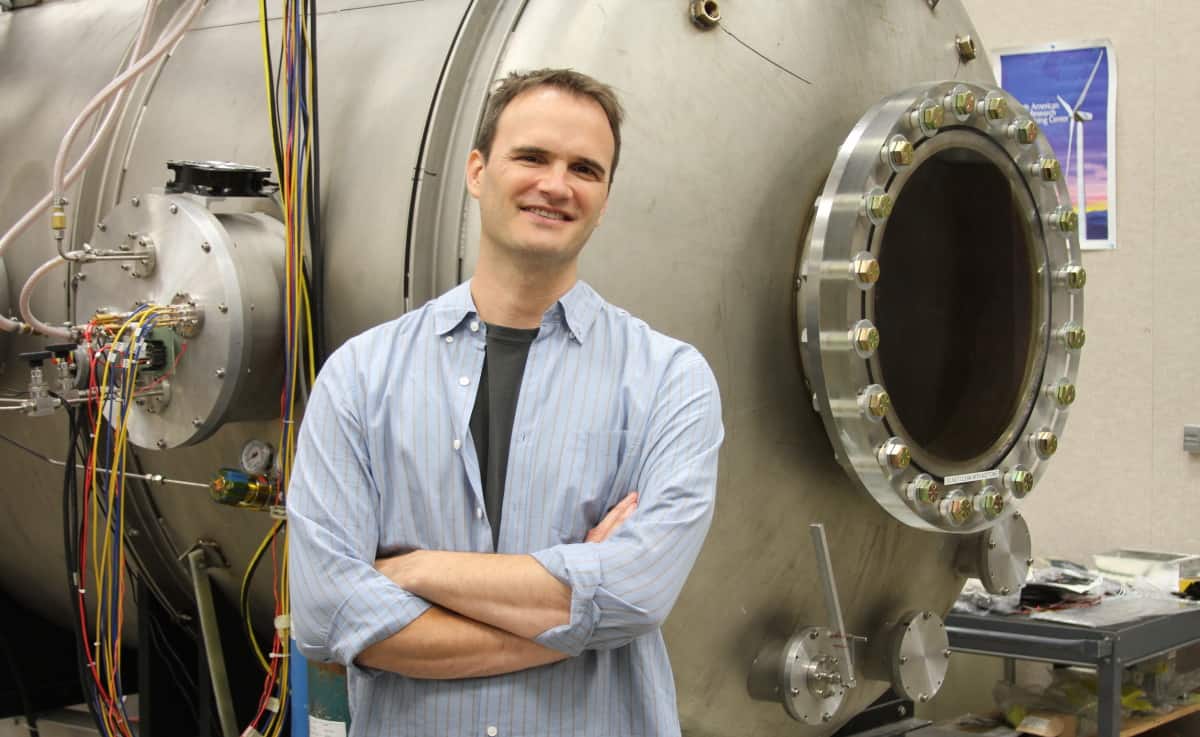
A team at the University of California, Los Angeles (UCLA), working with researchers from China and Canada, has developed a portable, air-fed cold atmospheric plasma (aCAP) device for such applications. In a proof-of-concept study, described in Science Advances, the aCAP device inhibited tumour growth and improved survival in mice following cancer surgery.
One major advantage of the team’s aCAP device is that it uses ambient air as the source gas to generate the cold plasma discharge, in contrast to conventional CAP systems that require bulky pressurized gas supplies. It can also be powered by batteries. This greatly reduces cost and complexity, and increases the feasibility of use in the operating suite as well as remote locations throughout the world.
Low-energy lightning
Plasma, an ionized gas, is the primary state of matter in stars, and comprises over 99% of the visible universe. Plasma made from air consists of many reactive species, radicals, electrons and photons. Lightning, a visible form of plasma, is a naturally occurring electrostatic discharge between two electrically charged regions that produce a giant arc of electricity with gigajoule energy in the ambient air.

Led by co-principal investigators Richard Wirz, director of the UCLA Plasma and Space Propulsion Laboratory, and Zhen Gu of the Zhejiang Laboratory of Systems and Precision Medicine at Zhejiang University Medical Center, the researchers designed the portable aCAP device around the concept of reducing the energy regime of lightning from gigajoules to joules. They achieved this by adjusting the voltages and distances between the device’s electrodes. The small arcs between these electrodes ionize ambient air that is fed through the device, resulting in a near-room-temperature jet of cold atmospheric plasma.
The team hypothesized that the local application of aCAP on residual tumour cells in a surgical cavity would induce a high level of reactive oxygen species (ROS) and reactive nitrogen species (RNS) in the tumour microenvironment. ROS and RNS are known to induce cancer immunogenic cell death and release tumour-associated antigens in situ, evoking effective anti-tumour immunity.
Cancer cell kill
The researchers first tested their prototype aCAP device in vitro with breast cancer and melanoma cells. They detected increased concentrations of ROS and RNS cells in the cells and the culture media, which caused potent tumour-killing effects.
Next, they used the device to treat the surgical cavity following resection of 400 mm3 breast tumours in mice. After surgery and application of aCAP (for 1, 2, 3 or 4 min) to residual tumour cells, they detected increased levels of calreticulin, an indicator of immunogenic cell death. The researchers used a thermal camera to monitor temperature in the aCAP-treated areas, reporting that no significant temperature changes occurred in and adjacent to the treated tissue.
To mimic residual microtumours, the researchers deliberately left 2–5% residual tumour after surgery, and monitored tumour regrowth. The mice that had surgery plus aCAP treatment showed significantly improved control of tumour regrowth compared with those that only underwent surgical excision.
Longer aCAP treatment correlated with better outcomes: over 40% of the mice survived for at least 60 days when treated with 4 min of aCAP. Co-lead authors Guojun Chen and Zhitong Chen suggest that extending the duration of aCAP treatment or performing repeated treatments could further enhance its therapeutic efficacy.
Microneedle patch combines cold plasma and immunotherapy to treat melanoma
“Our portable aCAP device for postsurgical cancer treatment simplifies CAP equipment configurations and more broadly facilitates its applications in medicine. We anticipate that this treatment approach is also applicable to other types of solid cancer,” note the authors. They add that aCAP treatment could possibly be combined with cancer immunotherapies, such as immune checkpoint blockade, to further improve therapeutic outcomes.
“We are planning to improve the form, function and ease-of-use of the device, while continuing with further studies to determine modes of operation that are most effective with mouse models and then larger animals,” says Wirz. “This will be a joint collaboration by our team at UCLA, Zhejiang University, McGill University, and the National Innovation Center for Advanced Medical Devices in Shenzhen. If successful, we will want to advance to human studies.”