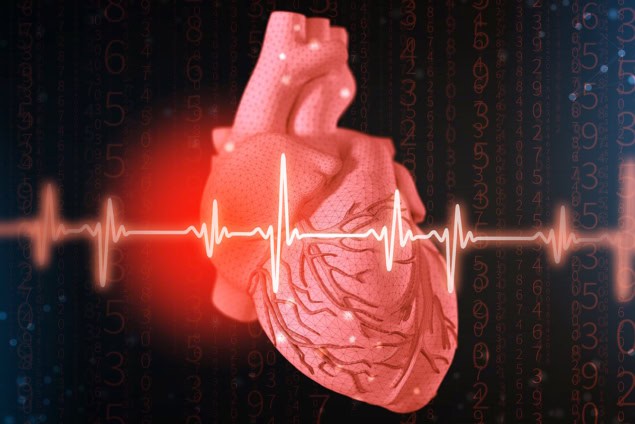
Evaluating electrocardiogram (ECG) traces using a new deep-learning model known as EchoNext looks set to save lives by flagging patients at high risk of structural heart disease (SHD) who might otherwise be missed.
SHD encompasses a range of conditions affecting millions worldwide, including heart failure and valvular heart disease. It is, however, currently underdiagnosed because the diagnostic test for SHD, an echocardiogram, is relatively expensive and complex and thus not routinely performed. Late diagnosis results in unnecessary deaths, reductions in patient quality-of-life and an additional burden on healthcare services. EchoNext could reduce these problems as it provides a way of determining which patients should be sent for an echocardiogram – ultrasound imaging that shows the valves and chambers and how the heart is beating – by analysing the inexpensive and commonly collected ECG traces that record electrical activity in the heart.
The EchoNext model was developed by researchers at Columbia University and NewYork-Presbyterian Hospital in the US, led by Pierre Elias, assistant professor at Columbia University Vagelos College of Physicians and Surgeons and medical director for artificial intelligence at NewYork-Presbyterian. EchoNext is a convolutional neural network, which uses the mathematical operation of convolution to generate information and make predictions. In this case, EchoNext scans through the ECG data in bite-sized segments, generating information about each segment and subsequently assigning it a numerical “weight”. From these values, the AI model then determines if a patient is showing markers of SHD and so requires an echocardiogram. EchoNext learns from retrospective data by checking the accuracy of its predictions, with more than 1.2 million ECG traces from 230,000 patients used in its initial training.
In their study, reported in Nature, the researchers describe running EchoNext on ECG data from 85,000 patients. The AI model identified 9% of those patients as being in the high-risk category for undiagnosed SHD, 55% of whom subsequently had their first echocardiogram. This resulted in a positive diagnosis in almost three-quarters of cases; double the rate of positivity normally seen in first-time echocardiograms.
EchoNext also outperformed 13 cardiologists in making diagnoses based on 3200 ECGs by correctly flagging 77% of structural heart problems while its human colleagues were only 64% accurate – a result so good that it shocked the researchers.
“The really challenging thing here was that from medical school I was taught that you can’t detect things like heart failure or valvular disease from an electrocardiogram. So we initially asked: would the model actually pick out patients with disease that we were missing? I have read more than 10,000 ECGs in my career and I can’t look at an ECG and see what an AI model is seeing,” enthuses Elias. “It’s able to pick up on different sets of patterns that are not necessarily perceptible to us.”
Elias instigated the EchoNext project after an upsetting incident in which he was unable to save a patient transferred from another hospital with critical valvular heart disease because they had been diagnosed too late. “You can’t take care of the patient you don’t know about. So we said: is there a way that we can do a better job with diagnoses?”
EchoNext is now undergoing a clinical trial, based in eight hospital emergency departments, that ends in 2026. “My number one priority is to produce the right clinical evidence that is necessary to prove this technology is safe and efficacious, can be widely adopted and has value in helping patients,” says Elias.
The heart of the matter: how advances in medical physics impact cardiology
He stresses that it is still early days for all AI technologies, but that even in these trial phases EchoNext – which was recently designated a breakthrough technology by the US Food and Drug Administration (FDA) – is already improving patient lives.
“It’s a really wonderful thing that every week we get to meet the patients that this helped. Our goal is for this to impact as many patients as possible over the next 12 months,” states Elias, adding that since EchoNext is successfully detecting 13 types of heart disease, a similar system should be useful in other healthcare domains too. “We think these kinds of AI-augmented biomarkers can become something that is routinely ordered and used as part of clinical practice,” he concludes.