The combination of gadolinium-loaded nanoparticles and monochromatic X-rays completely destroyed tumour spheroids within three days after 20 to 60 minutes of irradiation in a laboratory setting in Japan. The technique, which selectively amplifies the effect of radiation delivered to a tumour site, could eventually pave the way for a new type of cancer radiotherapy, according to researchers from Kyoto University’s Institute for Integrated Cell-Material Sciences (Sci. Rep. 10.1038/s41598-019-49978-1).
The research was conducted at Kyoto University and SPring-8, the largest third-generation synchrotron radiation facility in the world. The facility creates synchrotron radiation consisting of narrow, powerful monochromatic X-ray beams. These X-ray beams can be precisely tuned to target the K-shell of high-Z atoms, such as gadolinium, which causes ejection of inner K-shell electrons (K-edge activation) and triggers a series of events that releases Auger electrons. This approach, called photon activation therapy, has been shown to enhance DNA damage that can kill cells.

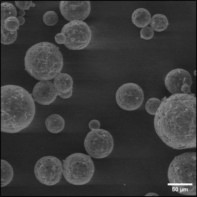
Principal investigator Fuyuhiko Tamanoi and colleagues hypothesized that nanoparticles loaded with high-Z atoms located close to the nuclei of cancer cells could improve this photon activation therapy. They selected gadolinium as the high-Z material because it can generate Auger electrons and cause DNA damage. After loading gadolinium into mesoporous silica nanoparticles, they added the nanoparticles into a culture media of human ovarian cancer cells and confirmed that the particles could enter the cells without causing toxicity.
The researchers next prepared tumour spheroids from ovarian cancer cells that express green fluorescence protein. Fluorescence imaging confirmed that the nanoparticles were uniformly distributed in the spheroids. They then irradiated tumour spheroids without and with varying levels of gadolinium using monochromatic X-rays at 50.0, 50.25 and 50.4 keV.
Tumour spheroids containing 50 ng of gadolinium-loaded nanoparticles and irradiated with 50.25 keV X-rays broke up into pieces 72 hours after a 10 minute exposure. After 60 minute exposure, these spheroids were completely destroyed. Spheroids irradiated with 50.4 keV X-rays showed slightly less levels of destruction, while 50.0 keV X-rays caused almost no spheroid damage.
Tumour spheroids containing 10 or 20 ng of nanoparticles were only partially destroyed, and there was no damage at all when the nanoparticles did not contain gadolinium.
“Destruction of the tumour spheroids was exposure time dependent and was also dependent on the amount of gadolinium loaded to spheroids,” the researchers write. “The dramatic difference between the effect of 50.25 and 50.0 keV X-rays is consistent with the idea that the Auger electrons are exerting cellular effect.”
As for the slight difference in destruction efficiency between 50.25 and 50.4 keV, noting that similar levels of energy are likely to be absorbed, the researchers speculate that the energy release processes may have differing degrees of efficiency and/or that the energies of electrons released from the inner shell differ. “It is also interesting that tumour spheroids were broken into pieces after irradiation, which may suggest that the treatment has some effect on cell adhesion,” they write.
The researchers are hopeful that a compact X-ray generator capable of producing monochromatic X-ray beams in a clinical treatment facility will be developed for experimental and clinical use. They are now planning studies using animal model systems, Tamanoi tells Physics World. After this research is successfully completed, the nanoparticles will need to be approved for use in human clinical trials.
“My guess is that it will take more than five years to be able to use this technology in a clinic,” Tamanoi says. “But I would like to emphasize that our work opens up a possibility to develop a new type of radiation therapy. This could have a major impact on how radiation therapy is carried out.”