
Major epidemics, including SARS, Zika and Ebola, and pandemics such as H1N1 and COVID-19 have gripped the world in the last two decades. As infectious disease outbreaks emerge with increasing regularity, the need to expand viral diagnostic and surveillance testing capacity to contain epidemics and prevent pandemics becomes progressively evident. Researchers led by Dino Di Carlo and Sam Emaminejad from the University of California, Los Angeles (UCLA) have now developed a handheld viral diagnostic test based on a swarm of millimetre-sized magnets (termed “ferrobots”). The technology could significantly increase the throughput of disease testing, while minimizing costs and usage of scarce supplies.
Describing the diagnostic lab kit in Nature, the researchers outline the working principle and adaptability of the platform for multiplexed and pooled viral testing. They also report results from a clinical study using samples from individuals with COVID-19 symptoms. Comparing test results using the lab kit with the same samples tested for COVID-19 using the gold-standard reverse transcription-polymerase chain reaction (RT-PCR) assay revealed a test sensitivity of 98% and specificity of 100%.
Overcoming supply shortages and reducing cost
Among the options for viral diagnostic and surveillance testing, nucleic acid amplification tests (NAATs) show clear advantages over antigen- and antibody-based tests, in terms of sensitivity, specificity and the capability for rapid provision without prior generation of specific diagnostic antibodies. However, previous NAAT-based testing platforms were unable to perform the integrated liquid handling, analysis and automatic feedback processes needed to achieve flexible workflows and maximize disease screening efficiency.
To overcome this shortfall, the UCLA researchers created a palm-sized printed circuit board-based programmable platform that performs liquid handling and bioanalytical operations in a parallel manner. In contrast to previous methods, which required bulky, resource-intensive instruments, the miniaturized platform delivers substantial cost savings over a wide range of viral prevalence, while simultaneously offering high precision, robustness, adaptability and scalability.
“Our handheld lab technology could help overcome some of the barriers of scarcity and access to tests, especially early in a pandemic, when it is most crucial to control disease spread,” says Emaminejad. “And beyond its potential to address issues of short supplies and high demand, it could be broadly adapted to test for many types of diseases in the field and with lab-grade quality.”
Moving to multiplexed and pooled testing
The researchers developed a suite of operations to detect the presence of genetic material from a virus – in this case, SARS-CoV-2 that causes COVID-19. The circuit board controls a swarm of ferrobots to transport magnetized samples through the diagnostic NAAT workflow, including automated transportation, aliquoting, merging, mixing and heating of sample droplets to amplify the reaction product (DNA). Finally, the results are determined based on a colour change of a pH indicator, which enables a binary interpretation of the test, above or below a threshold, as positive or negative, respectively.
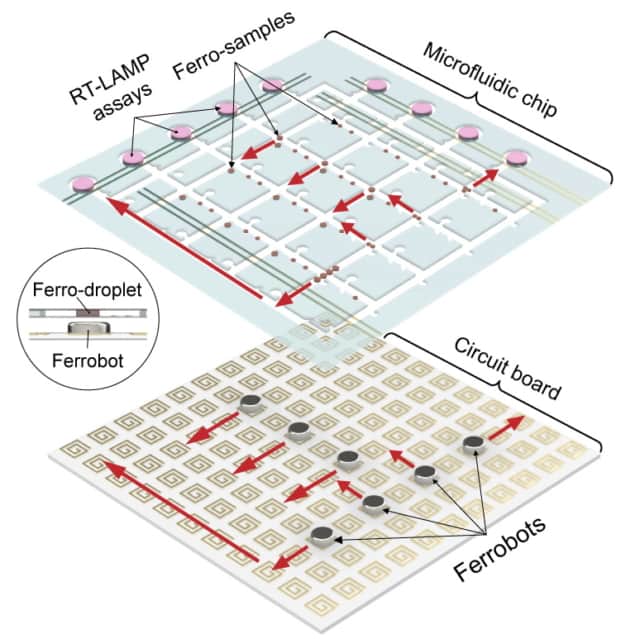
The UCLA researchers also demonstrated parallelization – moving many of the ferrobots at the same time using electromagnetic tiles in the circuit – as well as sequential task operations in a collaborative manner by each ferrobot (in coordination with the other ferrobots).
“This platform’s compact design and automated handling of samples enable easy implementations of pooled testing where you can test dozens of patient samples at the same time, and all with the same materials it currently takes to test just one patient,” says Di Carlo. “For example, you could test students in an entire college residence hall with just a few dozen test kits.”
Adaptable biosensor rapidly detects COVID-19 virus and antibodies
By implementing a pooled testing algorithm, which can test up to 16 samples in a single assay, the system requires much lower reagent costs than needed to test the samples individually. If the pooled test showed a positive result, a subsequent streamlined set of operations takes place within the platform until the actual positive samples are identified. Ultimately, the researchers note, chemical reagent costs could be reduced by 10 to 300 times depending on the viral prevalence.
As well as testing for several diseases simultaneously, the platform can analyse a large number of input samples in parallel and asynchronously as they arrive, avoiding wait times associated with batch processing. As such, the team concludes that this technology serves as a promising solution to increase testing capacity globally for epidemic and pandemic preparedness.




