An international research team has developed a pioneering radiotherapy technique that uses very high-energy electron (VHEE) beams to target tumours precisely. Proposed as an alternative to X-ray photons for radiation therapy, VHEE beams penetrate deep into tissue, but can also overexpose healthy tissue.
In this study, published in Nature Communications Physics, the researchers demonstrate how they overcame this problem by using a large aperture electromagnetic lens to focus a VHEE beam to an extremely small spot in tissue, concentrating the radiation dose into a small volume.
As study leader, Dino Jaroszynski, director of the Scottish Centre for the Application of Plasma-based Accelerators (SCAPA) at the University of Strathclyde, explains, this volumetric element can then be rapidly scanned over a tumour to “paint” all the areas of it, while minimizing the dose to healthy tissue.
“Taking the analogy of focusing sunlight using a hand lens, you will experience a serious burn if you place your hand at its focus, but only feel mild warmth away from the focus,” he says.
“Electron beams damage cancer cells in a very similar way to that of high-energy photons, which is the most common radiotherapy modality in the clinic,” Jaroszynski explains. “This is because high-energy electrons convert a large fraction of their kinetic energy to X-ray photons by bremsstrahlung, which triggers a cascade of electrons, positrons and photons, and also ionizes matter by inelastic collisions. These are what ultimately damage cancer cells, by directly ionizing the DNA or indirectly creating radicals that damage their DNA.”
Precise targeting
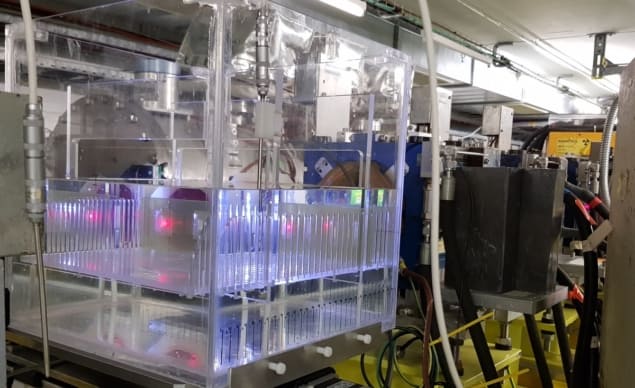
In experiments performed at CERN’s Linear Electron Accelerator for Research (CLEAR) facility, the team measured depth–dose profiles of 158 and 201 MeV electron beams focused into a water phantom. They demonstrated that the focused VHEE beams concentrated dose into a well-defined volume several centimetres deep into the phantom.
According to Enrico Brunetti, a research fellow at the University of Strathclyde, one key advantage of VHEE beams is that they can be produced at much lower cost than proton or ion beams. In addition, VHEE beams can reach deep-seated tumours with reduced susceptibility to tissue inhomogeneities.
“The range of a proton or ion beam depends on the integrated matter through which it passes. If there are voids, gas pockets or variable density material, the range will be uncertain. However, because VHEE beams are light-like, they will always deposit dose at the same spot, so are insensitive to the morphology of the tissue in their path,” Brunetti explains.
“The focusing method that we have developed enables the precise targeting of deep-seated tumours using VHEEs by concentrating dose into a small volume. This dose can be controlled, which may give an advantage in treating radiation-resistant tumours,” he adds.
According to Brunetti, the ability to deposit dose into a small spot can also benefit ultra-precision therapy, where there is a need to irradiate very small regions. In addition, the very low entrance dose and low distal and proximal doses of focused VHEE beams may help to minimize damage to healthy tissue and sensitive organs.
Next steps
Despite the clear advantages of the new technique, Brunetti is keen to stress that its use in clinical settings is some way off – and much work remains to be done on developing the laser and accelerator technology to make it suitable for clinical application.
“Our advice is to be patient and undertake further in vitro and in vivo studies, and eventual clinical trials. We have undertaken cell survival studies using VHEE beams and found them to be similar to X-ray photons. Interest in VHEE as a new modality is growing rapidly,” he says.
“If it can be demonstrated that VHEE beams, focused or not, give a clinical advantage, then research and development will accelerate. There would be a strong incentive to develop them to the point where they can be applied clinically because lives would be saved, and saved lives would translate into economic benefit,” he adds.

Very high-energy electrons could treat tumours deep within the body
Looking ahead, the next steps for the researchers are to implement symmetric focusing and investigate the use of larger bore focusing magnets to obtain even smaller focal spots, as well as to explore the use of a permanent magnet to focus the beam. They will also work alongside colleagues in Lausanne to investigate the use of VHEE beams to deliver FLASH radiotherapy (a cutting-edge technique that delivers high-dose-rate radiation in sub-millisecond time-scales to target tumours while sparing healthy tissue) in deep-seated tumours.
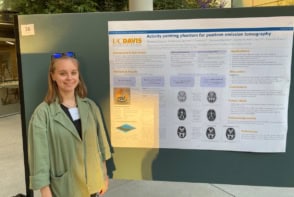
The team also plans to carry out in vitro and in vivo studies using facilities at Strathclyde, which include an EPSRC-funded research-focused medical beamline at SCAPA.
“Finally, we plan to investigate a new way of using VHEE beams to simultaneously apply radiotherapy and image the region around the tumour – this will give real-time imaging capability [and] is a very novel idea,” adds Jaroszynski.