A sampling and image-analysis method that spots and characterizes cancer cells in the blood has been developed by researchers in the US. The high-throughput technique quantifies the presence of androgen receptor (AR) proteins in cell nuclei — a prognostic indicator and measure of treatment efficacy for metastatic prostate cancer. Less invasive than a conventional biopsy, monitoring circulating tumour cells (CTCs) also provides a more representative picture of tumour properties in real time (Phys. Biol. 10.1088/1478-3975/ab073a).
Growth of metastatic prostate cancers is associated with the build-up of androgen receptors in cell nuclei. Usually restricted to the cell’s cytoplasm, these proteins are only transported into the nucleus when bound to the hormone androgen and a polymeric cellular component called a microtubule. In the nucleus, ARs bind to the DNA, activating a set of genes that promote tumour growth.
Most chemotherapy strategies for prostate cancer aim to prevent the activation of these genes by excluding ARs from the nucleus, which they achieve by inhibiting the function of microtubules. Measuring the presence of nucleic AR in cancer cells, then, offers a diagnostic tool and a way to monitor a treatment’s effectiveness.
The usual way to obtain cancer cells for such purposes would be to conduct a biopsy at the site of the tumour itself. For prostate cancer, this is an invasive procedure with a real risk of complications, and the information that it provides reflects just a single point in time and space. Seeking to improve on the convenience and diagnostic power of this technique, Daniel Worroll and colleagues at Weill Cornell Medicine developed a method to process and analyse liquid biopsies instead — blood samples that can be obtained easily and as frequently as treatment requires.
The researchers took blood samples from 15 patients being treated for metastatic castration-resistant prostate cancer (mCRPC), as well as four healthy donors whose blood was then “spiked” with a prostate-cancer cell line. First, they applied a cocktail of cell-specific antibodies to remove white and red blood cells from the samples, leaving a residue enriched in CTCs. The conventional way to isolate CTCs is to capture them directly using a cancer-specific cell-surface marker, but this method misses potentially important cancer cells in which the marker is absent.
“The biological relevance of CTCs that do not express traditional epithelial markers is something that requires more research,” says Worroll. “Based on other groups’ results, the hypothesis is that those tumour cells that lose epithelial markers may have a higher metastatic potential and be more resistant to chemotherapy.”
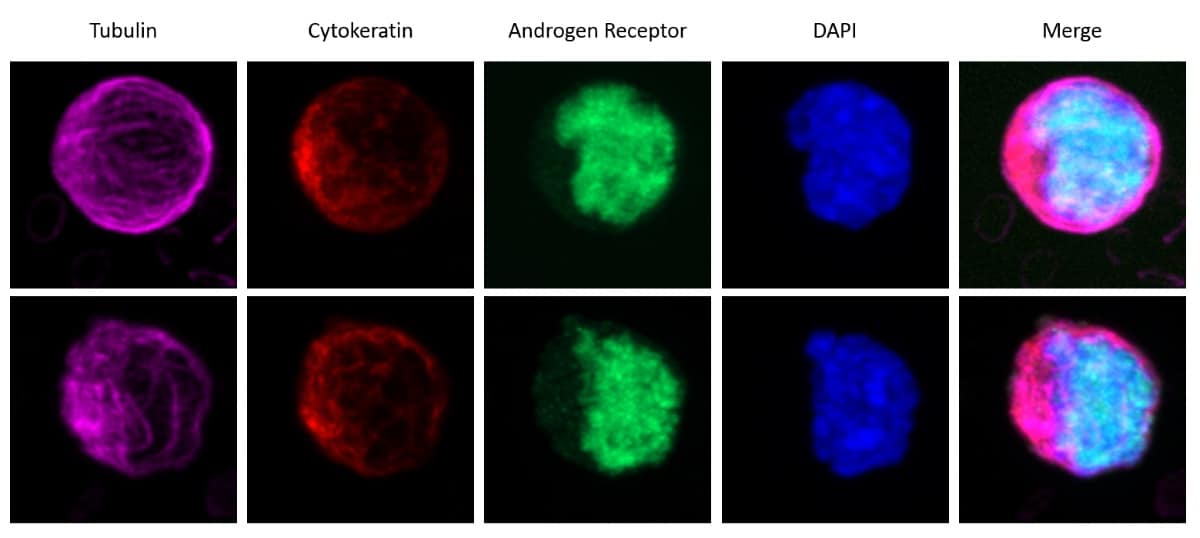
Next, the researchers stained the samples with a range of fluorescent antibodies that highlighted certain cellular components. This allowed the first step of the image-analysis process, in which an algorithm classified CTCs based on cell shape, size and fluorescence profile. Using a higher-resolution image of the same sample, the algorithm then identified the nuclei of individual CTCs, and determined the ratio of AR-related fluorescence in and outside of the nucleus.
Taking this ratio as a measure of AR nuclear localization, the researchers compared the results with the patients’ therapy outcomes. Patients who responded the least to chemotherapy tended to be those whose CTCs showed a greater quantity of nuclear AR. The explanation for this, Worroll and colleagues suspect, could imbue the technique with additional clinical value.
Although ARs rely on the presence of microtubules to access the cell nucleus — making them susceptible to treatments that target this vector — an AR variant exists that is not so dependent. Lacking the molecular structure that interacts with microtubules, variant AR-V7 gains entry to the nucleus by another (currently unknown) route, and is associated with a chemotherapy-resistant form of prostate cancer. The researchers measured the expression of AR-V7 messenger RNA in CTCs and found that the variant was more likely to be present in those cells with more nuclear AR.
“With multiple studies showing a zero-response rate of AR-V7-positive patients to AR-targeted therapies, detection of AR-V7 mRNA status prior to initiation of these therapies would have an obvious clinical impact,” says Worroll. “Furthermore, due to the non-invasiveness of liquid biopsies, longitudinal monitoring while on therapy for the emergence of AR-V7 would offer therapeutic benefit.”



