Biomedical sensors that actively monitor physiological signals from moving organs undergo large and cyclic deformations. To mechanically conform to the curvature of the organs and match their motion, such sensors typically feature thin designs to ease flexibility, and elastomer encapsulations to enhance stretchability.
To boost the mechanical performance of tissue-interfaced wireless biomedical devices, a research team at Singapore University of Technology and Design (SUTD) replaced the conventional metallic conductors in the antenna with Galinstan — a low toxicity gallium alloy that is liquid at room temperature.
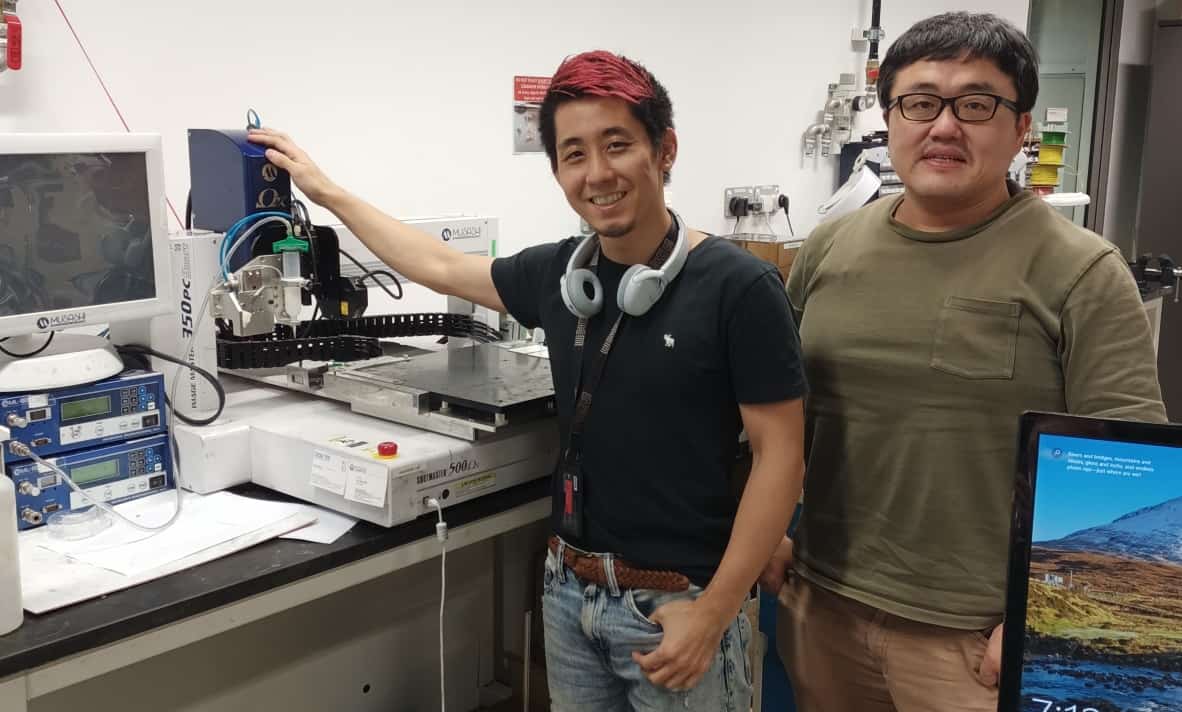
The 3D-printed microfluidic antenna, which the researchers describe in Advanced Materials, retains a high wireless power efficiency under extreme deformations and conformally adheres to fragile dynamic tissues, providing a thin, wireless sensing platform for health monitoring applications. “This technology will open up new opportunities for biological sensing, communication and therapeutics,” explains senior author Michinao Hashimoto.
Additively manufactured antennas
Challenging the existing liquid metal antennas, which have large, solid monolithic structures, Hashimoto’s team envisioned a soft, non-monolithic structure. To achieve this, the researchers employed a pneumatic silicone sealant dispenser to print the outline of a microchannel on a 7 µm-thick Ecoflex substrate, referred to as Ecoflex microsheet, which has similar elastic properties to biological tissues. After embedding a set of light-emitting diodes (LEDs) and a jumper wire into the device, they added a free-standing Ecoflex microsheet to seal the outline, resulting in an empty microfluidic channel.
To aid in the Galinstan injection process, the team used a rigid sacrificial layer of poly(vinylalcohol) — a water-soluble polymer — as a removable mechanical support to enable smooth liquid metal flow in the microchannels, thereby closing the electrical circuit and powering the LEDs. The resulting fluidic antenna operates close to the standard near-field communication frequency (13.56 MHz) with low energy loss.
Resilient electromagnetics
For stretchable electronics that include solid antennas, wavy and serpentine conductor patterns help to increase the overall stretchability. However, the range is still limited by the yield strain of the metallic conductor. Liquid metal, however, offers unlimited strain, making it an enticing choice for sensors that will experience large deformations.
The researchers report that the Galinstan antenna can experience up to 200% tensile strain, match a 3 mm radius of curvature and withstand a 180o twisting angle while maintaining a low energy loss. Repetitive tensile strain tests revealed no degradation in the antenna’s energy efficiency or meaningful shift in its operating frequency, highlighting the stability of the design. They note that pressing the antenna, however, could cause irreversible microchannel collapse if the pressure exceeds 90 kPa.
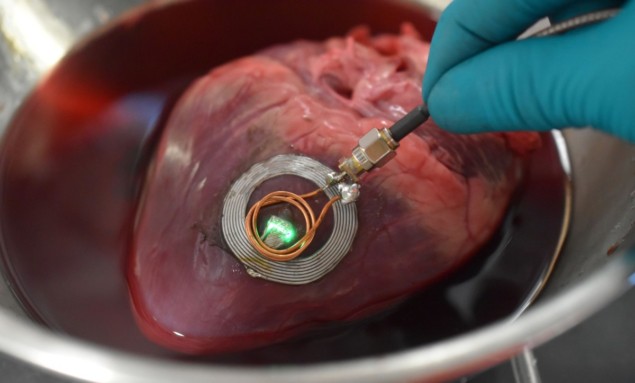
To secure the Galinstan antenna onto soft tissues, the team coated the tissue—antenna interface with a 650 nm-thick layer of the bio-adhesive polydopamine. This increased the adhesion energy, removing the need for sutures that could injure the tissue. Experiments on a porcine small intestine and heart, and a chicken leg revealed that the surrounding environment detuned the antenna and lowered its efficiency. However, it maintained sufficient performance to power the device’s LEDs.
“We believe this work covers the need for minimally invasive implantation of biodevices on fragile tissues such as the brain, liver and kidney,” says first author Kento Yamagishi, who plans to use this technology for future in vivo implantable studies in small animals.



