Mammography is a widely employed and effective tool for early detection of breast cancer, but dense breasts pose a significant challenge in cancer screening. Not only does dense breast tissue increase the risk of developing breast cancer, the high proportion of fibrous and glandular tissue can mask the presence of a tumour on a screening mammogram.
As a result, supplemental breast imaging modalities are often advised for women with dense breasts. Such tests, breast MRI in particular, add significantly to the cost of cancer screening. This is especially problematic considering that about 40% of the screening population have heterogeneously dense breasts and about 10% of women have extremely dense breasts.
Low-dose positron emission mammography (PEM) is a novel molecular breast imaging technique that could potentially replace or supplement mammography. With this in mind, researchers in Canada have compared the performance of PEM and breast MRI in identifying breast cancer and determining its local extent in 25 women recently diagnosed with breast cancer. They report the findings of their clinical study in Radiology: Imaging Cancer.

Historically, molecular breast imaging has not been used for clinical breast imaging due to the high radiation dose that it delivers to the breasts and surrounding organs. The use of an organ-targeted PET system – the Radialis PET Imager – to perform PEM could eliminate this concern. The Radialis uses coincidence detection of emitted gamma photons, eliminating the need for collimation (required for gamma camera-based molecular breast imaging) and enabling the use of radiation doses comparable to those of mammography.
PEM technology offers the high sensitivity of breast MRI but with the advantage of being lower in cost. Its effective radiation dose is comparable to that of traditional digital mammography and lower than digital tomosynthesis. In addition, PEM overcomes tumour masking issues associated with high breast density, delivers fewer false positives than mammography, and doesn’t require breast compression during the exam.
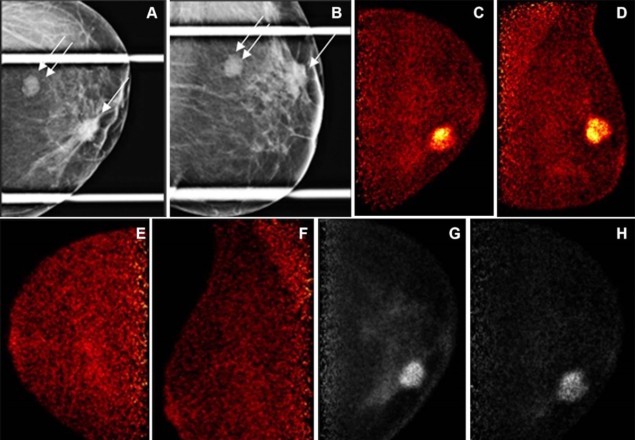
Principal investigator Vivianne Freitas, from the University of Toronto’s University Health Network, Sinai Health and Women’s College Hospital, and colleagues imaged the study participants 1 and 4 h after injection of 37, 74 or 185 MBq of the radiotracer 18F-fluorodeoxyglucose (18F-FDG). Similar to mammography, they acquired PEM images in standard craniocaudal and mediolateral oblique views.
Two breast radiologists blinded to the cancer location performed a per-lesion-visual assessment of the acquired images, recording the morphology of any observed lesions. Low-dose PEM identified 24 out of 25 known malignant lesions (determined by histopathology) compared with 100% for MRI, failing to detect a single 38-mm lobular cancer. MRI identified 13 additional lesions, eight of which were false-positives, while PEM detected six, one of which was a false-positive, demonstrating PEM’s lower false-positive rate of 16% versus 62% for MRI.
The researchers note that PEM’s low dose of 37–185 MBq produced diagnostic-quality images corresponding to a radiation exposure of 0.62–0.71 to 1.24–1.42 mSv. The low dose of the PEM device approached the mean total effective dose of two-view bilateral full-field digital mammography (about 0.44 mSv), was similar to contrast-enhanced mammography (0.58 mSv) and less than the combination of mammography and digital breast tomosynthesis (0.88 mSv).
“For screening, PEM’s ability to perform effectively regardless of breast density potentially addresses a significant shortcoming of mammography, particularly in detecting cancers in dense breasts where lesions may be obscured,” says Freitas. “It also presents a viable option for patients at high risk who are claustrophobic or who have contraindications for MRI.”
Freitas notes that while the full integration of PEM into clinical practice is yet to be confirmed, these preliminary findings are promising, particularly as they demonstrate PEM’s ability to detect invasive breast cancer with low 18F-FDG doses. “This marks a critical first step in its potential future implementation in clinical practice,” she says.
Wearable coil vest could change the game in breast MRI
The researchers have now started a pilot study to evaluate whether liquid biopsy findings can be matched to images obtained by PEM in women at high risk of breast cancer. Participants have blood taken for a liquid biopsy test and a PEM exam following injection of 74 MBq of 18F-FDG, before undergoing an MRI-guided biopsy for a suspicious breast lesion.
The team will evaluate data from the two exams to determine whether any novel findings on tumour fragment size and patterns, mutational signatures, variants or epigenetic changes identified from liquid biopsy correlate with the characteristics of the PEM images. If correlations between the two are identified, the researchers plan to conduct additional studies to evaluate whether these techniques can help refine screening investigations and reduce unnecessary biopsies.




