
Tumour hypoxia is associated with poor clinical outcome following radiation or chemotherapy in cancer patients. Measuring tumour oxygenation prior to or during therapy could help select the most appropriate treatments, as well as identify poor response earlier than currently possible, enabling effective changes in treatment regime.
Hypoxia is typically defined as oxygen tension (pO2) of less than 10 mmHg. One way to measure this in vivo is to insert oxygen-sensing microelectrodes into the tumour tissue. However, such measurements are invasive, limited to accessible organs, may modify the tumour microenvironment and are not amenable to repeated measurements.
An alternative approach is diffuse reflectance spectroscopy (DRS), which provides a non-invasive way to evaluate oxygenation in accessible tumours (skin or oral cavity, for example). As such, researchers from the University of Arkansas are investigating the use of DRS to measure sO2 – the average oxygen content bound to haemoglobin in the blood vessels. Their aim: to show that DRS can provide reliable in vivo measurements of tumour hypoxia (J. Biomed. Optics 23 067001).
“The main advantage of using DRS is its non-destructive and non-invasive nature,” explains lead author Narasimhan Rajaram. “Using a pen-shaped probe that is usually compatible with the working channel of endoscopes and laryngoscopes, it should be possible to interrogate tissue non-invasively and get a quantitative measure of tumour hypoxia.”

Optical approach
DRS works by illuminating the tissue-of-interest with 400-650 nm light and using the reflected light signal to quantify the underlying scatterers and absorbers. Since DRS is sensitive to the absorption of oxygenated and deoxygenated haemoglobin, it can quantify the amount of oxygenated haemoglobin to total haemoglobin content. DRS thus provides a measure of both sO2 and the total haemoglobin content (THb).
In this study, the team used a portable DRS system comprising a halogen lamp for illumination, a USB spectrometer for spectral acquisition, and a bifurcated optical probe for light delivery and collection. The probe incorporates four illumination and five detector fibres at a source–detector separation distance of 2.25 mm, providing a sampling depth of about 1.8 mm.
The researchers acquired DRS spectra from two different human head-and-neck cancer xenografts (radiation-resistant SCC-47 and radiation-sensitive SCC-22B cell lines), using an integration time of 100 ms and a wavelength range of 475 to 600 nm. They used a lookup table-based model to fit the acquired DRS spectra and extract wavelength-dependent absorption and scattering properties, and validated the results using immunohistochemical staining to quantify tumour hypoxic fraction (HF).
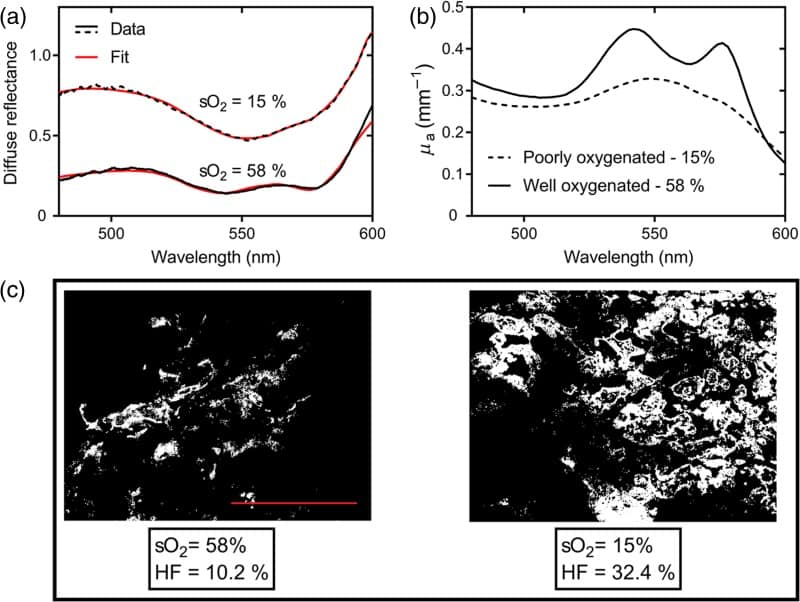
Fitting the DRS spectra for two excised tumours revealed sO2 values of 58% for one tumour and 15% for the other. For the oxygenated (58%) tumour, the absorption spectra exhibited the classic double peaks of oxygenated haemoglobin (542 and 577 nm), while the poorly oxygenated (15%) tumour showed a single peak corresponding to deoxygenated haemoglobin. Immunohistochemistry images of the HF confirmed that the tumour with higher sO2 had less hypoxic tissue than the low-sO2 tumour.
The researchers determined that HF was negatively correlated with sO2, and correlated with THb, indicating that DRS measurements of vascular sO2 and THb provide reliable indirect measures of tumour oxygenation. Specifically, they note that very low values of sO2 and THb can indicate highly hypoxic and poorly perfused tumour.
“Measuring a tumour’s response to therapy with diffuse reflectance spectroscopy is our clinical goal,” says Rajaram. “The oxygenation levels in a tumour prior to and post-radiation can be key biomarkers of radiation response of failure, which explains the current work with radiation-resistant and sensitive cell lines.”
Rajaram and colleagues are now investigating whether they can predict radiation resistance in the tumours when they are treated with radiation. “We are also working with collaborators at University of Arkansas for Medical Sciences, Little Rock, to run pilot studies with the probe in patients with head-and-neck cancer,” he tells Physics World.



