Radiation therapy is commonly employed as a primary or adjunct treatment for brain tumours. However, neurocognitive impairment after brain radiotherapy is a known problem that restricts its use. The ability to limit dose to brain regions associated with cognitive performance may help minimize treatment-related loss of cognitive functioning, ultimately improving patients’ long-term outcomes and quality-of-life.
Functional MRI (fMRI) provides a means to identify brain regions to selectively protect during radiotherapy. Previous research in this area has focused on task-based fMRI of language and sensory networks. Now, a team from University of Maryland School of Medicine has investigated the feasibility of incorporating resting-state fMRI data into radiation treatment plans for patients with primary brain tumours (J. Med Imaging Radiat. Sci. 10.1016/j.jmir.2018.09.003).
“Resting-state fMRI provides the ability to collect information on how the brain is functionally communicating without requiring the participant to perform a task, which he or she may be unable to do due to limited cognitive abilities or causing further fatigue to the ailing patient,” explains first author Chandler Rhodes. “Additional benefits include the ability to look at multiple brain networks (such as language, vision, hearing and memory) in a single 6–10 min scan, as well as the ability to collect this information on a standard MR scanner without the additional equipment needed for task-based fMRI.”
Seek and avoid
Rhodes and colleagues used resting-state fMRI to identify the brain’s default mode network (DMN), a set of cortical regions associated with cognitive functioning. Damage to this neural network can lead to reduced cognitive performance, and the researchers propose that protecting the DMN during radiation delivery could minimize side effects such as memory loss.
To investigate this premise, they retrospectively incorporated fMRI data from the DMN into the radiation treatment plans of nine patients with primary brain tumours. All patients had previously received standard-of-care radiotherapy using either intensity-modulated or 3D conformal radiotherapy.
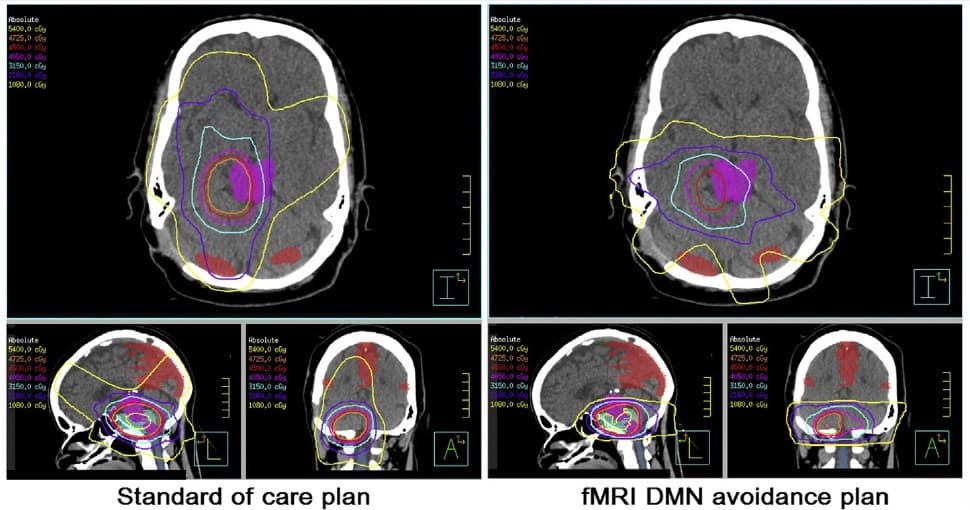
For each participant, the researchers performed 3T MRI to obtain resting-state fMRI data and structural images. They overlaid the fMRI networks of the DMN onto each individual’s structural image, imported this into a treatment planning system and contoured the DMN onto the planning CT scan. Finally, they generated a second treatment plan that reduced dose to the DMN while maintaining dose to the planning target volume (PTV) and not increasing dose to organs-at-risk (OARs).
The team successfully extracted fMRI maps of the DMN and created DMN avoidance plans for all participants. In all cases, the new plans reduced the dose to brain areas related to cognitive functioning compared with the standard-of-care plans. On average, the avoidance plans reduced the maximum dose to the DMN by 12% and the mean dose by 20%.
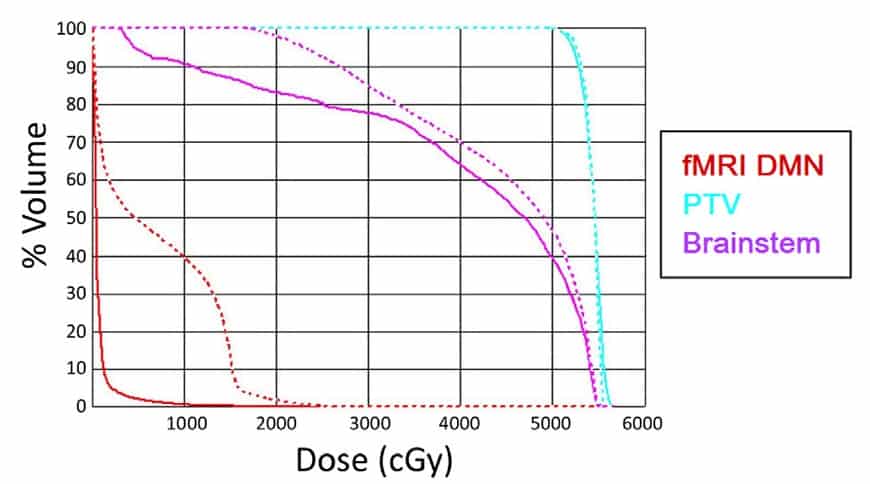
Importantly, these dose reductions were achieved without compromising dose coverage of the PTV or significantly increasing dose to any of the OARs (brainstem, spinal cord, lenses, retina, lacrimal glands, cochlea, optic nerves and optic chiasm). The avoidance plan also reduced the dose non-PTV and non-OAR brain tissue.
Potential benefits
To estimate the relative benefit, in terms of improved cognitive function, for patients treated with the DMN avoidance plan, the team used a normal tissue complication probability (NTCP) modelling approach. Multivariate analysis showed that age, smoking history, tumour histology, and volume of DMN receiving 10 Gy (DNM10Gy) were all predictive of memory loss.
Using these variables, the researchers identified two logistic regression models that successfully predicted memory loss: one with age and DNM10Gy as variables; and the second with tumour histology and DNM10Gy as variables. Incorporating these two models into the NTCP calculation enabled them to calculate the probability of developing memory loss.
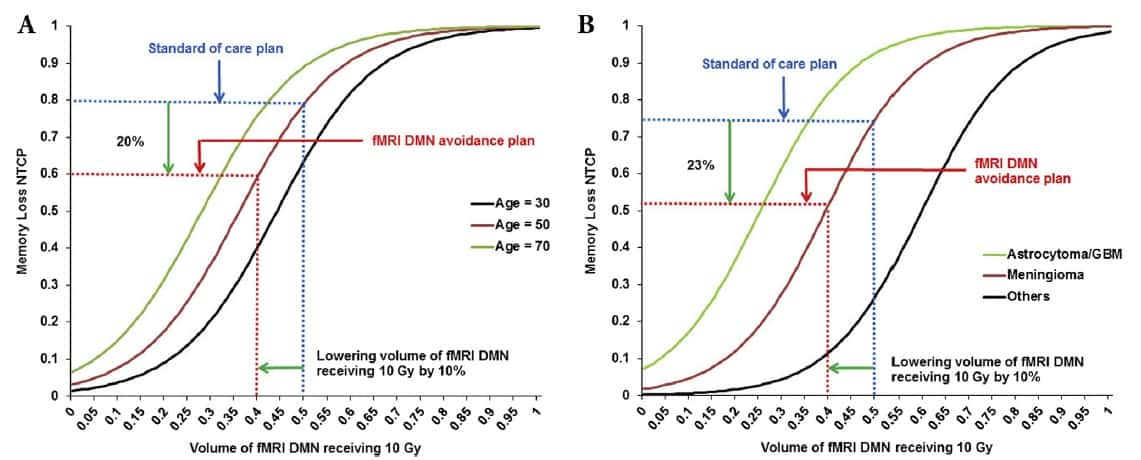
On average, the fMRI DMN avoidance plan reduced the DNM10Gy from 50% to 40% compared with the standard-of-care plan. This dose reduction lowered the probability of developing memory loss by 20% for 50-year-old patients, for example, and by 23% for patients with meningioma.
The authors conclude that incorporating DMN derived from resting-state fMRI into radiation treatment plans is feasible and can reduce dose to the DMN without significantly affecting dose to the PTV or OARs. This approach may significantly reduce toxicity in brain regions associated with cognition.
They caution, however, that as the potential benefits were only estimated using models, the study does not prove that reducing dose to the DMN actually reduces the cognitive decline that often follows radiation treatment. They suggest that the clinical impact of this reduction in DMN dose needs to be further evaluated in a rigorous clinical trial.
The team also plans to test the proposed approach with proton therapy. “Since proton therapy has the potential to provide superior dose distribution in terms of sparing the fMRI DMN, our approach may demonstrate even more benefits with proton therapy,” says co-author Howard Zhang. “We are also planning a prospective study to assess the effectiveness of incorporating functional imaging into radiation therapy in terms of patient outcomes,” adds senior author Rao Gullapalli.



