RSNA 2019, the annual meeting of the Radiological Society of North America, is taking place this week, with some 50,000 attendees heading to Chicago to learn about the latest advances in radiology research. Here’s a small selection from the studies presented at the conference.
Focused ultrasound may enable Alzheimer’s therapies
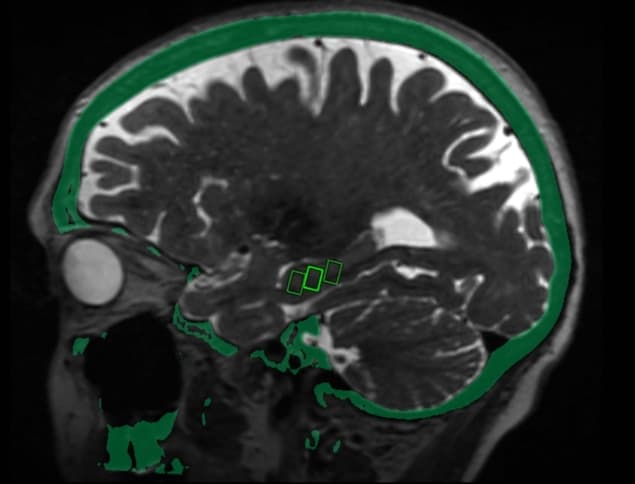
There currently is no effective treatment for Alzheimer’s disease, in part because the blood–brain barrier (BBB) prevents potential medication from reaching targets inside the brain. Animal studies have shown that pulses of low-intensity focused ultrasound (LIFU) can reversibly open this barrier to enable targeted drug and stem-cell delivery. In a clinical trial led by Ali Rezai, director of the WVU Rockefeller Neuroscience Institute, researchers at three sites delivered MRI-guided LIFU to brain sites critical to memory in three women with early-stage Alzheimer’s disease.
The treatment uses a helmet containing over 1000 ultrasound transducers that’s placed over the patient’s head after they are positioned in the MRI scanner. Each transducer delivers ultrasound targeted to a specific area of the brain. Patients also receive an injection of microbubble contrast agent. As ultrasound is applied, the bubbles oscillate and transiently loosen the BBB. Post-treatment MRI confirmed that the BBB opened in target areas immediately after treatment and then closed within 24 hours. Patients received three treatments at two-week intervals and experienced no adverse effects.
Research so far has focused on the technique’s safety; in future, the team intends to study LIFU’s therapeutic effects. “We’d like to treat more patients and study the long-term effects to see if there are improvements in memory and symptoms associated with Alzheimer’s disease,” says co-author Rashi Mehta. “As safety is further clarified, the next step would be to use this approach to help deliver clinical drugs.”
AI helps detect heart disease on lung cancer screens
Low-dose chest CT is employed for lung cancer screening in high-risk people, such as long-time smokers. Such CT scans can also visualize coronary artery calcification (CAC), a measure of arterial plaque used to help decide whether to prescribe cholesterol-lowering medication. But despite its value, CAC is not routinely determined in CT lung screens, as the measurements require dedicated software and add time to the interpretation.

Researchers from the Cardiovascular Imaging Research Center at MGH and the Artificial Intelligence in Medicine Program at Brigham and Women’s Hospital have developed a technique that uses deep learning to automatically measure CAC on chest CT images. “If our tool detects a lot of coronary artery calcium in a patient, then maybe we can send that patient to a specialist for follow up,” says lead author Roman Zeleznik.
The researchers trained their deep learning system on cardiac and chest CTs with manually measured CAC values, and then tested the algorithm on CT scans from thousands of heavy smokers. They found that deep learning-derived CAC scores corresponded closely with those of human readers. There was also a significant association between deep-learning scores and cardiovascular death over follow-up of 6.5 years.
The deep learning system adds no time to the exam and can be used on almost every chest scan to generate clinically relevant information for a large number of patients. “There’s information about cardiovascular health on these CT scans,” says co-senior author Michael Lu. “This is an automated way to extract that information, which can help patients and physicians make decisions about preventative therapy.”
Brachytherapy effectively treats skin cancers
High-dose-rate (HDR) brachytherapy offers excellent cure rates and cosmetic outcomes when treating skin cancers in elderly patients, according to a study presented by Ashwatha Narayana from Northern Westchester Hospital. Squamous cell carcinoma (SCC) and basal cell carcinoma (BCC), the most common skin cancers, are usually treated by surgery or external-beam radiotherapy. But for elderly patients, who don’t heal well and may have additional medical problems, surgery may not be the best option.

“If the affected area is the tip of the nose, ear or on the eyelid, multiple surgeries and skin grafting may be required,” explains Narayana. External-beam radiotherapy, meanwhile, can be too lengthy and painful for elderly patients. It also exposes healthy tissue around the lesion to radiation, which can increase side effects. “Brachytherapy delivers a higher dose of radiation directly to the tumour while sparing healthy tissue nearby,” he adds.
HDR brachytherapy delivers a precise radiation dose to tumour cells via catheters implanted into a custom-fitted applicator. A treatment course comprises six three-minute sessions over two weeks. Patients have minimal recovery time and typically experience few or no side effects. In the study, radiologists used HDR brachytherapy to treat 70 patients with early-stage BCC and SCC. The patients had a total of 81 lesions on the nose, face, forehead, scalp, ear, neck and legs. The procedure provided a cure rate of 96% for SCC and 98% for BCC, with excellent cosmetic outlook in 90% of cases.
MRI-guided ultrasound ablates prostate cancer
Prostate cancer is the second-leading cause of cancer death in men, and treatment is challenging: surgery and radiation are not always effective and can cause serious side-effects. MRI-guided transurethral ultrasound ablation (TULSA) has emerged as a promising minimally invasive treatment option. TULSA delivers precise ultrasound doses to diseased prostate tissue while sparing surrounding healthy tissue, using a rod-shaped device inserted into the urethra. The device incorporates 10 ultrasound-generating elements that are automatically controlled to adjust the shape, direction and strength of the therapeutic ultrasound beam. The entire treatment takes place in an MRI scanner, providing real-time monitoring of the thermal dose and ablation efficacy.
In a new multicentre study, researchers used TULSA to treat men with localized low- or intermediate-risk gland-confined prostate cancer. They delivered ultrasound to the entire gland, in a treatment that took an average of 51 minutes. Overall, clinically significant cancer was eliminated in 80% of participants, with 72 out of 111 men having no evidence of any cancer after one year. Blood levels of prostate-specific antigen, a marker of prostate cancer, fell by a median of 95%. Patients had low rates of severe toxicity and no bowel complications.
“We saw very good results in the patients, with a dramatic reduction of over 90% in prostate volume and low rates of impotence with almost no incontinence,” says co-author Steven Raman from UCLA. “There are two unique things about this system. First, you can control with much more finesse where you’re going to treat, preserving continence and sexual function. Second, you can do this for both diffuse and localized prostate cancer and benign diseases, including benign hyperplasia.”



