Norovirus is the most common cause of gastrointestinal illness, with infection causing vomiting, diarrhoea and stomach pain. It is also extremely contagious. Made infamous by outbreaks on cruise ships, norovirus can also affect public water systems, schools and restaurants.
“It only takes a very small number of norovirus particles to cause an infection in humans, so we need a really sensitive detection method,” says Jeong-Yeol Yoon from the University of Arizona. “Also, scientists aren’t able to culture norovirus in the lab, and available antibodies to the pathogen aren’t very strong.”
As a result, detecting minute amounts of norovirus in water or food samples typically involves complicated concentration of viruses and/or amplification of genetic materials, which must be conducted in a lab by trained personnel. At the ACS National Meeting, held this week in San Diego, CA, Yoon described an inexpensive portable device that can detect just a few norovirus particles in water.
Yoon and colleagues have created a smartphone-based device that employs fluorescence imaging. Their technique uses a paper microfluidic chip, to which a water sample potentially containing norovirus is added. Next, the researchers add a suspension of fluorescent beads covalently linked to antibodies against norovirus, and the two liquids mix. If norovirus is present, the virus particles will bind to multiple antibodies, each of which is attached to a fluorescent bead. This binding causes the beads to aggregate and produce an intense fluorescent image.
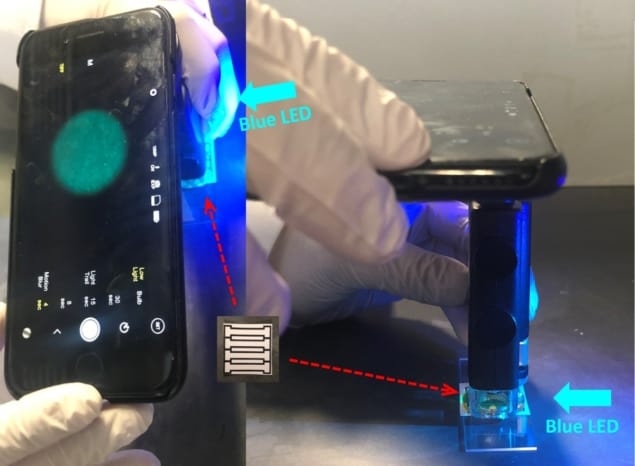
To visualize this fluorescence, the researchers converted a standard smartphone into a fluorescence microscope by attaching a commercial light microscope accessory, a separate light source and two band-pass filters. They also wrote software to analyse images of the microfluidic chip and calculate norovirus concentrations from the pixel count of the images.
“The lowest detection limit corresponded to about five or six norovirus particles per sample, so it’s very close to the single-virus level,” Yoon says. Because as few as 10 virus particles can cause illness in people, the new method is sensitive enough for practical applications.
Yoon and colleagues recently made the system more compact and handheld by enclosing the fluorescent microscope, light source and optical filters in a 3D-printed case. They also developed a cloud-computing app to analyse the large images and send the results back to the smartphone. In addition, they have found a way to concentrate samples within the paper chip so that they can analyse much larger sample volumes.
The device could detect miniscule amounts of norovirus in both purified water (as low as 1 genome copy/μl) and reclaimed wastewater (10 genome copies/μl). Yoon notes that tap water, however, was prone to error, likely due to chlorine affecting the assay. “We don’t think it will be a problem to treat the water to remove chlorine before performing our method,” he says.
Yoon envisions that staff at public water systems staff could use the smartphone-based device and app to check for norovirus in the water supply. It could also be deployed on cruise ships or used to rapidly test hundreds of wells on site without having to take samples back to the lab.



