Every part of our body needs oxygen to survive, produce energy and function. This is especially important after a potentially life-saving transplant, where the new organ needs to quickly establish a blood supply and get enough oxygen to start working well in its new host body. If not, the transplant may fail.
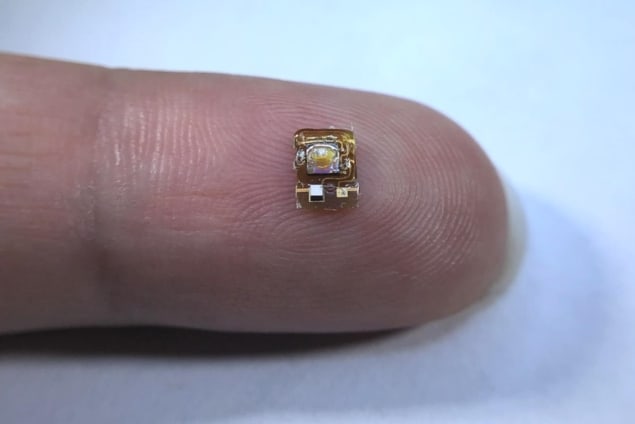
An innovative and minute new sensor developed by engineers at the University of California, Berkeley can detect how much oxygen an organ is getting from inside the body and give doctors an early warning of danger for the transplanted organ. In the future, the sensor could even be adapted to measure a huge variety of other important biological parameters.
Getting sound information
“It’s very difficult to measure things deep inside the body,” says Michel Maharbiz, from UC Berkeley and the Chan Zuckerberg Biohub. This is especially tough when what needs to be seen is not a visible structure, but the amount of a molecule, such as oxygen, inside a tissue.
No imaging technique currently available can tell us directly how much oxygen an organ is receiving. Other methods to measure this are limited by the need for wired connections to the organ, the ability to make observations only close to the skin, or the inability to provide real-time data. Maharbiz and his team used their expertise in making tiny implantable devices that communicate with the outside world to offer a new route to solving this problem. Their device is less than half-a-centimetre in length – smaller than the average ladybird – and can be placed directly onto the organ.
The team used ultrasound – high-frequency sound waves that are safely and routinely used in medicine for imaging – to power and receive information from their device. Unlike light waves, the ultrasound can propagate easily through tissue and allow communication even deep within the body.
Inside the device is an oxygen sensor incorporating an LED light source, a custom integrated circuit with a light detector, and an oxygen-sensing film containing luminescent ruthenium dyes. The amount of oxygen present changes the properties of light emitted by the ruthenium dye, which the device measures and reports back out of the body via ultrasound waves.
“The device demonstrates how, using ultrasound technology coupled with very clever integrated circuit design, you can create sophisticated implants that go very deep into tissue to take data from organs,” says Maharbiz.
Measurements more than skin deep
In their study, reported in Nature Biotechnology, the researchers showed how their device worked effectively when implanted into a sheep, giving similar readings to a wired probe but without requiring a direct connection. They also demonstrated how the sensor functioned deep beneath tissue – performing measurements through 10 cm of pig muscle.
Whilst there is still significant work to be done to translate these successful tests into clinical use, the researchers are optimistic about the impact of their miniature sensor. “One potential application of this device is to monitor organ transplants, because in the months after organ transplantation, vascular complications can occur, and these complications may lead to graft dysfunction,” says postdoctoral researcher Soner Sonmezoglu, who led the effort to incorporate oxygen sensing into this device and designed the electronic controls to operate and read out the device.
In 2019, 17.5 organ transplants were carried out globally every hour. The ability to monitor the status of those organs more closely could help doctors spot problems before they become critical and make crucial life-saving interventions.
The researchers believe their work could have many other applications, by adapting the sensor to measure other important biological markers. “By just changing this platform that we built for the oxygen sensor, you can modify the device to measure, for example, pH, reactive oxygen species, glucose or carbon dioxide,” Sonmezoglu explains. “Also, if we could modify the packaging to make it smaller, you could imagine being able to inject it into the body with a needle, or through laparoscopic surgery, making the implantation even easier.”