Astronomers use adaptive optics to see past the Earth’s atmosphere, which distorts celestial objects and makes them appear to twinkle. A new technique called adaptive optics gonioscopy (AOG) applies similar principles to image the human eye.
Researchers at Indiana University published the results of their proof-of-concept study in Translational Vision Science & Technology (10.1167/tvst.8.5.5).
Glaucoma: origins and impact
The clinical motivation for developing this new imaging technique is glaucoma, an eye disease currently affecting 76 million people worldwide. Interventional procedures, such as laser therapies or surgery, have mixed outcomes, and the physiology of the disease is poorly understood.
In an eye that functions normally, clear fluid circulates throughout, supplying nutrition and maintaining the eye’s shape. The eye’s trabecular meshwork – a series of sequentially smaller pores – acts like a sieve, allowing fluid to drain properly and regulating pressure.
The trabecular meshwork is altered in glaucoma. Fluid no longer drains properly and intraocular pressure, a risk factor for glaucoma and its progression, rises.
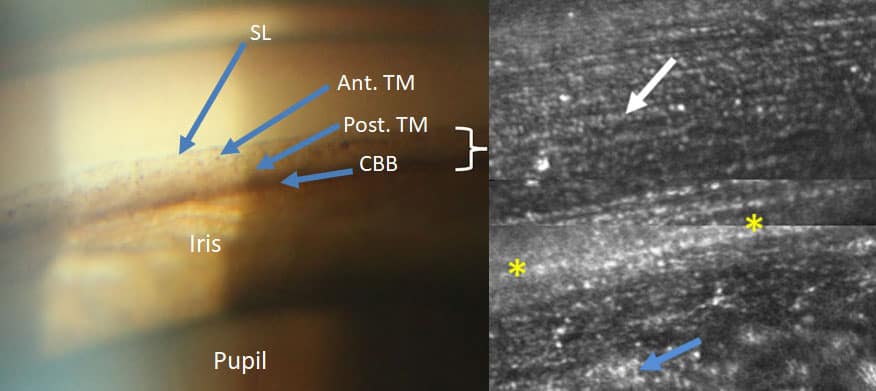
“As a result, the trabecular meshwork is an important structure to study, but direct imaging has been difficult,” says Brett King, lead author on the study. “AOG allows us to overcome the natural, near total internal reflection in this region and the differences in index of refraction between the eye’s cornea and the air.”
To see or not to see with AOG
King’s team successfully used AOG to visualize the trabecular meshwork at near cellular-level resolution in a proof-of-concept study with nine individuals (seven healthy volunteers and two with pigment dispersion syndrome, thought to be a precursor to glaucoma). This high-resolution visualization is a vast improvement over current clinical imaging methods, which only allow clinicians to determine the relative level of pigmentation of the trabecular meshwork and evaluate an individual’s risk of developing certain types of glaucoma.
The AOG technique requires an existing adaptive optics system for imaging the retina, which includes a wavefront sensor and deformable mirror. The wavefront sensor measures optical aberrations while the deformable mirror corrects for them. The researchers added cameras to assist clinicians in placing the modified gonioscopy lens on a patient’s eye and added a head mount to reduce patient motion.
Shooting for the stars
One challenge that the researchers faced was knowing what it was they were looking at. “As AOG imaging of the trabecular meshwork had not been performed before, we had difficulty at first realizing where we were and what structures we were seeing,” says King.
The researchers compared their images to pathology images that were often distorted from surgical or post-mortem artefacts. They also tested the technique with a model eye used to train surgeons.
King and colleagues are now building a new device to image even deeper within the eye and account for anatomical differences between individuals. They hope that this work will improve our understanding of age-related and pathological changes that occur in the human eye, as well as responses to pharmacological and surgical interventions.



