When a medical device such as a pacemaker or neurostimulator is implanted within a person’s body, the immediate question is how long its battery will function before requiring surgical removal and replacement.
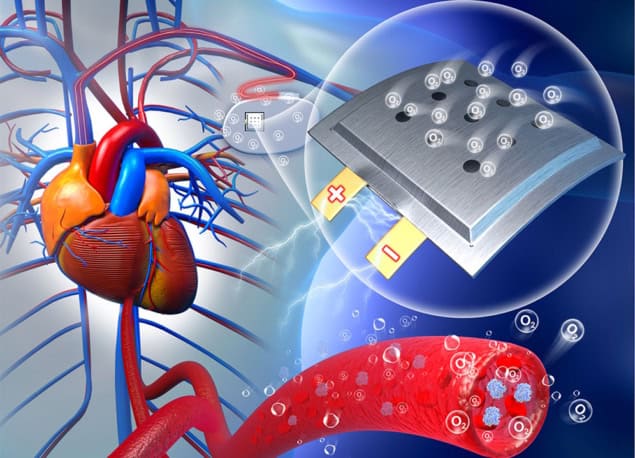
Researchers in China have developed an implantable Na–O2 battery with an open cathode structure that runs on oxygen circulating in the body, potentially removing the limit on battery life. In tests on laboratory rats, the team showed that the proof-of-concept design delivers stable power and has excellent biocompatibility.
Metal–O2 batteries have been previously tested for potential implantable use, but have encountered challenges. Their design requires an open cathode architecture to absorb oxygen from body fluids, and any discharge products created must be easily metabolized by the body during battery cycling. In addition, all components must be biocompatible and the battery must be flexible enough to enable stable contact with soft tissues.
The novel battery consists of a nanoporous gold catalytic cathode, an ion-selective membrane that acts as the separator and an anode made from a sodium-based alloy (NaGaSn). Nanoporous gold, which demonstrates excellent biocompatibility, has previously been used as a cathode in metal–air batteries to provide the oxygen reduction reaction. In the Na–O2 battery, oxygen continuously supplied from body fluids is reduced through the catalysis of the nanoporous gold during discharging.
The ion-selective membrane prevents body fluids from reaching the anode, though the team note that the NaGaSn alloy electrode possesses high safety and stability in water. The entire battery is encased within a soft and flexible porous polymer film.
Principal co-designers Yang Lv, Xizheng Liu and Jiucong Liu, of Tianjin University of Technology, initially conducted in vitro experiments, after which they implanted the battery under the skin on the backs of laboratory rats. After 24 h, they observed an unstable discharge voltage plateau. However, after two weeks of implantation, the battery was able to produce stable voltages of between 1.3 and 1.4 V, with a maximum power density of 2.6 µW/cm2.
“We were puzzled by the unstable electricity output right after implantation,” explains Xizheng Liu in a press statement. “It turned out that we had to give the wound time to heal, for blood vessels to regenerate around the battery and supply oxygen, before the battery could provide stable electricity. This is a surprising and interesting finding because it means that the battery can help monitor wound healing.”
The rats healed well after battery implantation, with the hair on their backs completely regrown after four weeks. Importantly, blood vessels regenerated well around the cathode, providing a continuous source of oxygen. Quantitative analysis confirmed that the number of capillaries around the battery was the same in rats with implanted batteries and control animals without batteries. In fact, the number of capillaries gradually increased with prolonged implantation time.
The researchers assessed the biocompatibility of the implanted battery through biochemical and immunohistochemical analyses. None of the rats developed inflammation around the batteries. Byproducts created by the chemical reactions of the battery, including sodium ions, hydroxide ions and low levels of hydrogen peroxide, were easily metabolized in the kidneys and liver. Upon completion of the study four weeks later, the rats did not experience any negative physiological effects, suggesting that the implanted battery has potential for practical applications.

Speaking the language of cells to power tiny machines
While the energy generated by the proof-of-concept battery is not sufficient to power medical devices for human use, the results demonstrate that harnessing oxygen in the body for energy is possible. Xizheng Liu advises that the team’s next plan is to improve the battery’s energy delivery by exploring more efficient electrode materials and optimizing the battery structure and design. “We think that the battery will be easy to scale up in production, and choosing cost-effective materials will further lower the cost to produce.”
The researchers note that, in addition to having a novel architecture with the ability to generate extremely high energy densities, the battery’s oxygen concentration can be controlled precisely. This capability may expand its use to therapeutic applications, such as starving cancerous tumours of oxygen or converting the battery energy to heat to destroy cancer cells. Future research initiatives will include evaluating other uses for this promising implantable battery.
The research is reported in Chem.



