Dementia with Lewy bodies (DLB) is the second most common cause of degenerative dementia in elderly patients. Small amounts of protein – Lewy bodies – clump together within nerve cells in the brain. As a result, communication between cells is significantly reduced over time, eventually leading to cell death.
There are several symptoms that lead to the diagnosis of DLB. These include significant variations in the patient’s attention and alertness and rapid eye movement. But many DLB symptoms are also commonly seen in Parkinson’s disease (PD) and Alzheimer’s disease (AD). Although the diagnostic sensitivity for DLB has increased over time, the clinical detection rate is considerably lower than that at autopsy, attributed to the misdiagnosis of DLB as AD. This can significantly impact the clinical management of each individual patient.
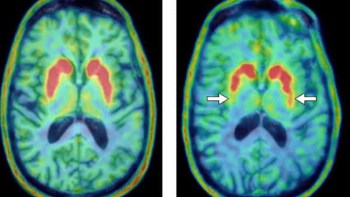
One approach considered to help differentiate between DLB, PD and AD is SPECT imaging using the radiotracer 123I-FP-CIT. This established imaging technique is able to detect nigrostriatal degeneration – depletion of dopamine-producing neurons in the brain’s striatum – a common indicator of both PD and DLB, but not seen in AD.
Upon injection, the 123I-labelled tracer binds to dopamine transporters located on dopamine-producing neurons. As 123I decays, it releases high-energy gamma photons that are detected by the SPECT system. A reconstructed image of the spatial distribution of 123I can be used to highlight presynaptic neuron degeneration, shown via reduced tracer uptake. Previous studies have reported abnormal binding findings as indicative of probable DLB.
Current methods, however, including qualitative visual evaluation of SPECT scans, have proved unable to accurately differentiate DLB from PD. To address this, a research team headed up by Francisco Oliveira at Champalimaud Centre for the Unknown has re-evaluated the diagnosis of patients with dementia using quantitative analysis of 123I -FP-CIT SPECT images, comparing the results with final diagnosis at autopsy.
Quantitative evaluation
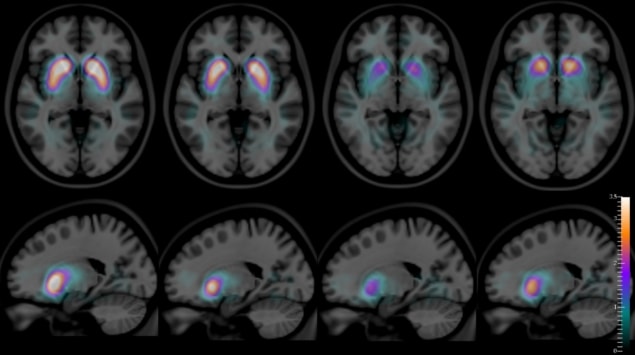
The researchers studied 123I-FP-CIT SPECT scans of 36 patients and their histopathological diagnoses at autopsy. They performed quantitative analysis on the SPECT images to compute the binding potential in two structures in the brain’s striatum – the caudate and the putamen – and the putamen-to-caudate ratio for all cases. The binding potentials represent the signal intensity in the target region compared with the background reference intensity.
The group performed statistical analysis to compare the binding potentials and putamen-to-caudate ratio across all three patient groups. Additionally, they evaluated the ability of these parameters to differentiate between different dementia types, using receiver operating characteristic curve analysis.
In comparison with diagnosis from visual assessment, quantitative evaluation of the binding potentials and putamen-to-caudate ratio showed significant improvement in differentiating DLB from AD and PD. The caudate binding potential helped separate patients with DLB from those with AD with high accuracy (94%).
The group established that although visual evaluation can accurately discriminate between patients with DLB and AD, this was not the case with DLB and PD. However, Oliveira and colleagues identified that, using the putamen-to-caudate ratio, DLB could be differentiated from PD patients with an accuracy of 94%.
The authors believe that “being able to quantitatively make these distinctions between diseases is crucial”, as misdiagnosis of DLB can have a significant impact on patient management.
Future implementation
The ability to accurately discriminate between different types of dementia using the computed binding potentials and putamen-to-caudate ratio from 123I-FP-CIT SPECT imaging is clear. “Our findings may have a significant impact both for patients and caregivers,” claim the researchers. Patients with DLB can be highly sensitive to some specific types of medication, which can lead to accelerated deterioration. By accurate diagnosis of DLB, the administered medication could be tailored accordingly.
In the future, the researchers aim to utilize the putamen-to-caudate ratio to distinguish, as early as possible, patients with DLB from those with Parkinson’s disease with dementia. This may ensure that an appropriate treatment strategy is implemented. “Nevertheless, further studies need to be done to prove our hypothesis and also to ascertain whether changes in putamen-to-caudate ratio would be sensitive in predicting cognitive decline,” say the researchers.
The researchers published their findings in the Journal of Neurology, Neurosurgery and Psychiatry.