Members of the Hassanpour Lab envision a world where, in less than 30 seconds, a pathologist will know the diagnoses and prognoses for one of the deadliest cancers in the western world.
In collaboration with pathologists from Dartmouth-Hitchcock Medical Center (DHMC), Saeed Hassanpour’s research team has developed and validated a deep-learning model that quickly assesses histopathology slides from lobectomy procedures, during which a lobe of the lung is surgically removed. Their tool promises to reduce pathologists’ workload and the subjectivity of visual analysis of heterogeneous histologic patterns. The findings were published in Nature Scientific Reports (10.1038/s41598-019-40041-7), and their code is publicly released on GitHub.
Deep learning for diagnosis and prognosis
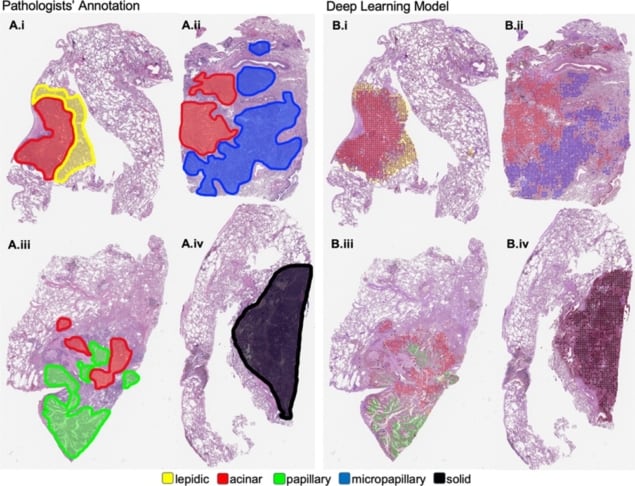
Lung adenocarcinoma is the most common type of lung cancer and one of the most lethal. Pathologists classify and grade histopathology slides from lobectomy procedures under a microscope according to their histologic patterns, or subtypes. Accurate interpretation of predominant and subtle minor patterns is important because these can determine a patient’s diagnosis, prognosis and health outcomes.
Determining at what point lung adenocarcinoma becomes invasive is a key challenge for pathologists’ visual analyses of histopathology slides.
“Some [histologic] patterns are more aggressive,” explains Laura Tafe, one of three pathologists involved with the study. “Even a small component of micropapillary pattern, as little as 5–10%, is important to identify because these patients are at increased risk for having disease spread to the regional lymph nodes.”
Intermingling invasive and non-invasive patterns, as well as inflammation or scarring, can also hinder accurate quantification of patterns and contribute to variation in pathologists’ analyses.
Neural networks, explained
Deep learning, a subset of machine learning, “is not currently in any position to replace pathologists or radiologists,” says Hassanpour. Still, deep-learning neural networks may be able to assist pathologists by automating time-intensive, difficult tasks. Last year, Hassanpour’s team set about using such a deep-learning neural network to assist pathologists’ analyses of lobectomy slides.
Collect, scan, train, validate
The researchers collected and scanned 422 histopathology slides procured from lobectomy procedures at DHMC. Three pathologists digitally annotated five histologic patterns and benign tissue on 245 whole-slide images.
The researchers trained a convolutional neural network to identify major and minor histologic patterns on these 245 slides. To improve the model’s performance, they broke up pathologists’ annotations into square, fixed-size patches, oversampled patches from less prevalent patterns, neutralized colour differences between slides, and performed image augmentation to generate a larger number of samples.
After training, the researchers evaluated the model against pathologists’ performance using 143 whole-slide images. Results suggested that the deep-learning neural network performs on par with the pathologists, while both pathologists and the model found detection of minor patterns challenging.
Toward clinical implementation
Hassanpour and Tafe see great promise in their deep-learning model for pathologists and patients alike. For example, it could pre-screen lung adenocarcinoma cases, aiding in pathologists’ visual inspection and interpretation by identifying aggressive minor histologic patterns. The team also plans to conduct a clinical trial incorporating education and trust-building to determine whether the deep-learning model improves outcomes in patients.
“Collaborations such as this between pathologists and data scientists are essential to advancing the field of oncology. Our expertise is disparate, which perhaps is exactly why it can be so powerfully complementary,” Tafe says.