Stereotactic body radiation therapy (SBRT) is highly effective in targeting high dose to a tumour while minimizing radiation exposure to surrounding healthy tissue. But if the mean radiation dose reaching potentially cancerous tissues immediately surrounding the tumour is not high enough, a patient may be at risk for developing distant metastases.
A Canadian study of non-small cell lung cancer (NSCLC) patients suggests that irradiation of a secondary margin outside the planning target volume (PTV) of a tumour could dramatically reduce distant metastasis rates, without adverse consequences to patients (Radiother. Oncol. 10.1016/j.radonc.2018.05.012).
If these findings are independently confirmed, radiation dose escalation beyond the PTV may be beneficial. The researchers suggest the use of a secondary margin outside the PTV subject to a dose constraint of at least 20.8 Gy2 (where Gy2 is the equivalent dose delivered in 2 Gy fractions) to ensure the eradication of microscopic malignant cells.

In a prior investigation of SBRT outcomes of NSCLC patients, André Diamant from McGill University Health Centre had determined that radiation target volume size was inversely correlated with distant metastasis. Because this finding seemed counter-intuitive, Diamant and colleagues conducted a study to determine whether a correlation exists between the dose immediately outside the PTV and metastatic development in patients with stage 1 NSCLC treated with SBRT.
The researchers analysed the distant metastatic rate in 217 patients with a single primary tumour. The patients had received SBRT either at McGill University Health Centre (96 patients receiving 3D-CRT) or Centre Hospitalier de l’Université de Montréal (121 patients receiving VMAT). Radiotherap was planned using a PTV with a 3-5 mm extension margin to the internal target volume.
Distant metastases developed in 37 patients (17% of the total) at 10 different sites, and loco-regional failure in 26 patients (12%). Eighteen patients (8%) experienced radiation pneumonitis. The researchers determined that two years after treatment completion, 60% of patients who received a mean dose outside the PTV of lower than 20.8 Gy2 developed distant metastases. This compared with only 5% for patients who received a higher mean dose to the same region.
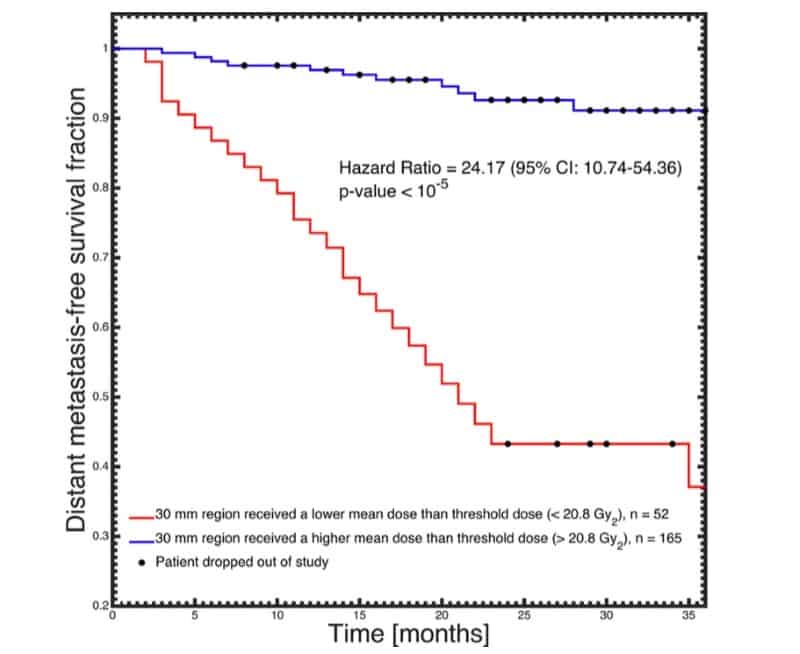
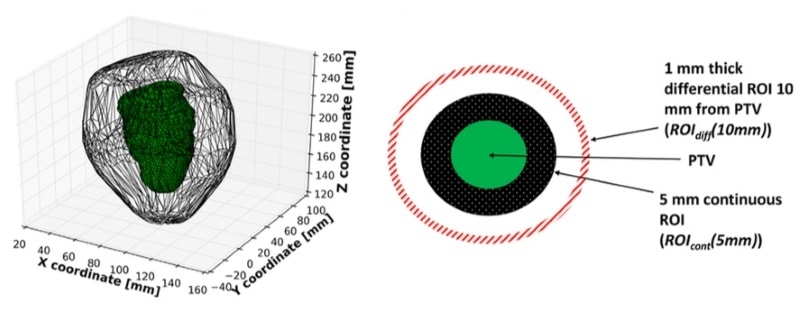
The researchers evaluated dose parameters in a region of varying size outside each patient’s PTV. The maximum difference in mean dose fall-off between the two groups (distant metastases versus no distant metastases) was 6.6 Gy2, at 16 mm away from the PTV. The authors suggest that ROIcont(30 mm), a shell-shaped region of thickness 30 mm outside the PTV, represents the region most indicative of the risk of distant metastasis. The mean dose received by this region had an area under the curve (AUC) of 0.82.
None of the dose coverage factors (homogeneity index, mean and median PTV) were predictive, nor were differences between planned and delivered dose distributions arising from patient setup error or movement.
The authors note that microscopic disease extensions, which have been reported at least 26 mm beyond gross tumour edges, were killed more efficiently by the higher mean dose. The immunosuppressive nature of radiotherapy may also have influenced the spread of microscopic tumour cells. This might explain the correlation with distant metastasis without seeing any correlation in loco-regional control.
“When it comes to dosimetric outcome analysis, the attention is often solely on the PTV, which is assumed to contain any and all microscopic cancer spread,” Diamant tells Physics World. “Our work indicates that perhaps more attention should be directed towards neglected regions that may contain otherwise unknown cancer cells. If confirmed independently, this calls for more advanced treatment planning strategies which take into account the biological tumour environment,”
“We are very interested in extending the analysis to other treatment modalities and/or cancer types. Additionally, we are actively researching the use of current artificial intelligence technologies to combine both image and dose information to predict oncological outcomes,” Diamant adds.



