Irina Grigorescu, a medical physicist at King’s College London, explains how artificial intelligence can transform medical physics
What benefits does AI bring to medical physics that other tools cannot?
Artificial intelligence (AI) is a constantly evolving discipline that could be of great scientific value to medical physics in three main areas. First, with most modern hospitals relying heavily on imaging to diagnose patients, AI could help busy staff to screen patients earlier and so manage their workloads more efficiently. If we had well-trained deep-learning models, then someone going in for, say, a magnetic resonance imaging (MRI) or computed tomography (CT) scan could immediately be flagged as a priority by the algorithm in case something suspicious is found. In fact, a group led by Ryan McTaggart from Brown University in the US has already developed a practical tool to quickly identify and prioritize patients with potentially life-threatening blockages to their blood vessels (Radiology 297 640). Such a tool would be impossible without AI technologies; instead, a radiologist would have to laboriously go through each image one by one.
Second, research has shown that deep-learning models can often reduce medical errors. In a paper published last year in Nature (577 89), for example, an AI system studying X-ray mammograms was shown to be better than human experts when it came to predicting whether or not a patient has breast cancer. More specifically, the model was found to be as good as two doctors looking at the images, and better at spotting cancer than a single doctor, while also reducing the number of “false-negative” results. Such systems will never replace medical staff, but would serve as an extra set of eyes, while also being able to work 24/7 without getting tired or making mistakes.
Finally, I believe that AI tools will soon be used in self-diagnostic applications. I can imagine doctors in a local GP clinic, for example, helping patients to monitor their health using their smartphones and to keep track of their physical condition – even diagnosing themselves when worried. Quite simply, AI software can do things that would be impossible with other tools in medical physics.
What are the disadvantages of using AI?
AI techniques are still in their infancy. Yes, they have shown great potential, and yes, they can already solve lots of tasks. But AI is not yet fully “intelligent”. One critical example is a 2019 study in the journal Jama Dermatology (155 1135), which showed that a deep-learning algorithm trained on skin-cancer images could be wrongly biased towards predicting melanoma. Such biases will have to be removed from our training datasets for the AI to become accurate enough for use in the real world.
Fighting algorithmic bias in artificial intelligence
Machine-learning techniques currently depend on high-quality datasets. Any bias introduced in the data could therefore be used as a “shortcut” for the algorithm to exploit. It’s a problem that extends beyond medical imaging. For example, with current technology, a self-driving car cannot accurately distinguish between a picture of a human and a real person on the road, which could lead to potentially disastrous outcomes.
The good news is that finding these vulnerabilities will let researchers maximize the capabilities of AI, and thereby improve our understanding of how they work and of how to develop new and better algorithms.
How do you use AI in your research?
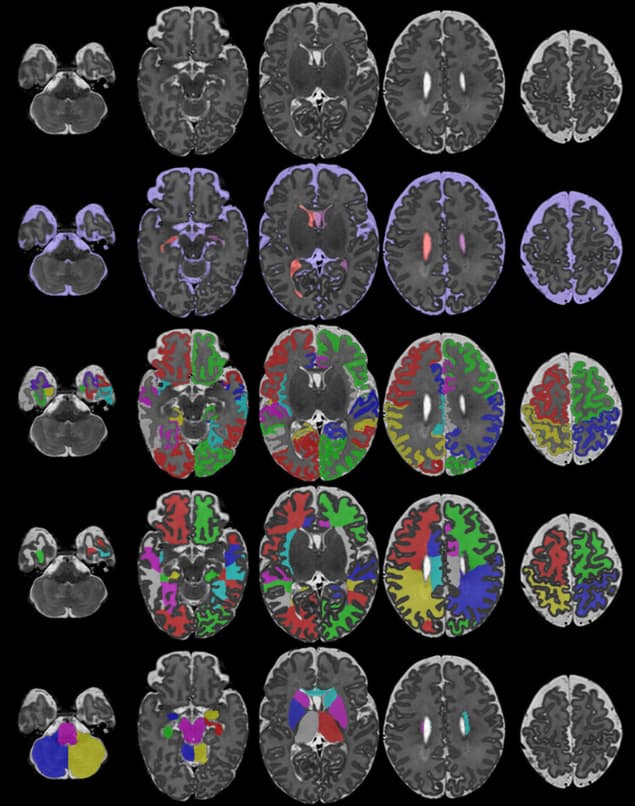
As part of my PhD, we are seeking to improve our understanding of how a baby’s brain develops during the first few weeks of its life. In particular, we are trying to characterize the developmental trajectory of a healthy brain by applying AI to MRI scans of babies acquired via the developing Human Connectome Project (dHCP), led by King’s College London, Imperial College and the University of Oxford. In my project, we are trying to create a “movie” of how a normal brain develops, but as we only have “snapshots” of different newborn babies at different ages, we first need to match similar anatomical areas of the human brain across all the different images and babies. It’s challenging work as the brain changes significantly during those vital first few weeks.
To achieve this goal, I am building a deep-learning framework that can take both structural and microstructural information of the brain and find these “anatomical correspondences” over time. By the end of my PhD in 2022 we hope to have a 4D model of brain development that can be used to detect abnormalities, predict developmental trajectories, and find if there are any anatomical regions in the brain that are important for normal development.

Along with Alena Uus and Maria Deprez, I am also using AI to automatically localize the foetus in MRI images of a mother’s uterus. The dataset is part of the iFind (intelligent Foetal Imaging Diagnosis) project, led by clinicians from King’s College London, St Thomas’ Hospital, Imperial College, the University of Florence in Italy, the Hospital for Sick Children in Toronto, Canada, and Philips Healthcare. In this work, not only do we try and detect the foetus in the images, but also its different organs, which will ultimately help improve the information available for clinicians to perform their diagnosis.
In what specific areas of medical physics will AI be most useful and most crucial in future?
One key example that comes to mind is the fastMRI challenge – a collaborative research project between Facebook AI Research and the NYU Langone Health medical centre in New York City, which was launched in 2018 to make MRI scans faster. For most patients, MRI scans are uncomfortable if they take too long. They’re also expensive. But by acquiring “under-sampled” images and using AI methods to reconstruct the data, the hope is that we can make scans up to 10 times faster.
At the same time, I believe that AI will soon be used to help radiology departments with management and planning. More specifically, I can envisage having an AI algorithm that can decide which tests a patient should have, and how a treatment should be personalized for each individual. Our imaging protocols could also benefit from this by training algorithms to predict the most effective and cost-effective ways of optimizing our current imaging protocols.
AI is here to stay – at least for the foreseeable future – and I think it will eventually become part of standard clinical practice. But as with all new technology, there is still much work to be done – and it will be vital to develop models that are ethical, accurate and trustworthy.



