Materials scientist Michele Barbour explains how the dental community is driving innovation in biomaterials with applications that stretch far beyond standard fillings and crowns
Dentists are fascinating people. Multiskilled and multidisciplinary by nature, these renaissance women and men of our time need to be consummate and compassionate communicators, able and adaptable scientists, and skilled and artistic creators. Dentists need excellent communication skills to advocate smoking cessation, counsel people on maintaining good oral health, and treat anxious patients with compassion and care. Because dental technologies and treatments are in a state of continual evolution, dentists must also be scientifically literate, critical thinkers; it is essential for clinicians to stay up to date with developments throughout their careers. Since dentists restore teeth that have become unsatisfactory for many reasons – including pain, loss of function, or simply being unsightly – they must be artistically as well as technically skilled, and able to intervene in an environment that is cramped and full of nerve endings. And contrary to what you might expect, their involvement in healthcare is not limited to tooth and gum care: dentists are in fact gatekeepers of whole-body health, as oral problems and symptoms sometimes indicate systemic health conditions.
Tough materials
For a materials scientist like me, though, the most fascinating thing about dentists is that, whether they realize it or not, they are discerning and meticulous materials engineers. Materials underpin so much of a dentist’s daily life: whether they are filling cavities; fitting dentures, crowns and sports mouthguards; or applying tooth-whitening treatments, many of their standard processes require polymers, ceramics, alloys or other advanced materials. Rarely will a dentist pass a day in the clinic without using some sort of material that must function in intimate contact with the hard and soft tissues of the mouth.
The strictures that dentistry places on these materials are also unusually tough. Like any biomaterial, a dental material must be biocompatible – that is, it must not elicit any adverse reaction, and it must be stable and maintain its function for the required period (which could be anything from a few minutes to the lifetime of the patient, depending on the application). But over and above those standard requirements, the material must also be able to survive in a hostile environment: the mouth. As well as constant moisture, parts of the mouth experience pH values that range from near-neutral to less than 3.0 (cranberry juice, for instance, has a pH of ~2.8); temperatures that run from close to 0 to around 60 °C; and pressures of tens of MPa in normal function. Natural tooth tissues – the enamel and dentine – are well equipped to withstand damp conditions with huge variations in force and temperature, but they are less able to cope with the modern low-pH diet, which is a comparatively recent addition in evolutionary terms. Indeed, the tendency of hydroxyapatite – a calcium-containing mineral that makes up 70% of the dentine and more than 90% of enamel – to break down in the presence of acids is known to be the root cause of tooth decay: the acids produced by plaque bacteria cause a slow but steady dissolution of tooth mineral, ultimately leading to the formation of a cavity.
The biomaterials used in dentistry must, therefore, be carefully engineered to be strong in compression, tension and flexure. They must not corrode or otherwise deteriorate when wet, and they must be able to resist frequent and rapid changes in temperature and pH. In recent years the commercial aspects of dentistry have also driven more stringent requirements regarding the physical appearance of the material. In colour, translucency and fluorescence, patients are increasingly demanding materials that are indistinguishable from the adjacent natural teeth, to the naked eye at least.
Freedom to choose
Of course, all of these materials come with a price tag, and those with the best balance of physical, mechanical, chemical and biological properties can be very lucrative for manufacturers. This drives innovation, because dental materials are big business: the global market for dental restorative materials and adhesives was estimated at just over $1bn in 2016, with a compound annual growth rate of more than 5%. Equally important is the fact that dentists are able to innovate; even dentists who work in publicly funded health systems have a degree of choice when selecting materials, and in private dentistry that choice is even wider. This means that dentists can be, and often are, early adopters of new technologies. It is thus in the interest of dental materials manufacturers to continually innovate and release new materials onto the market in a bid to capture this enthusiasm for the “new and improved”; complacency leads to loss in market share.

This combination of factors creates a niche occupation: the dental materials scientist. This is the niche I found myself occupying at the outset of my academic career 12 years ago. The dental sector appealed to me because I wanted the materials I develop to have a direct and near-term impact on people’s day to day lives – both the clinicians who use the materials and the patients who benefit from the clinician’s skill. I also came to appreciate the culture of progress and innovation that has grown up around dental materials owing to dentists’ opportunity to choose. This opportunity is significantly greater for dentists than it is for, say, orthopaedic surgeons or urologists, who have a more limited portfolio of materials to choose from when installing a hip implant or a urinary catheter (to take just two examples).
Over the past decade or so, the field of dental materials has seen several interesting developments. The mechanical strength of light-cured polymer composites – which are used to restore teeth in cases where a good aesthetic outcome is essential, for example if the teeth are near the front of the mouth – has improved considerably, and innovations in polymerization methods have reduced the amount of shrinkage usually associated with similar polymers. The field has also been rocked by the Minamata Convention, a legally binding treaty that commits signatories to ceasing the use of mercury across almost all industries. The convention has been signed by 84 countries, and its adoption puts amalgam, an important tool in a dentist’s armoury, under threat.
Smarter infection control
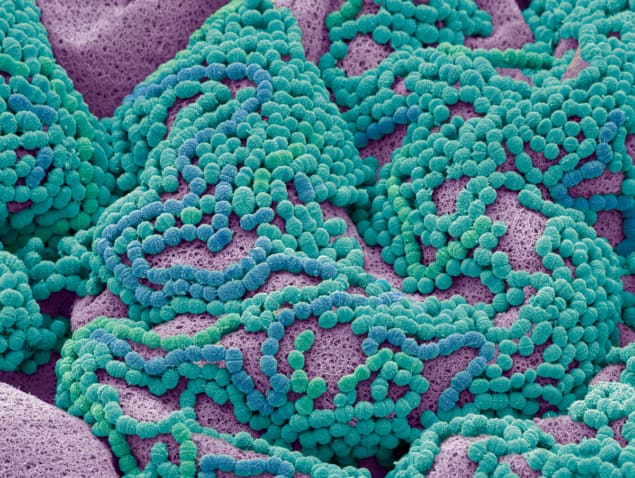
In my opinion, though, the most interesting developments have been in the field of antimicrobial dental materials, where my own research lies. The starting point for our work is a common and widely used antiseptic called chlorhexidine. Dentists use chlorhexidine as a multipurpose antimicrobial for treating gum disease and oral infections; it is also applied preventively before dental surgery. Other uses in the wider medical world include skin disinfection (again before surgery), combatting MRSA outbreaks in hospitals, and as a component of wound dressings for chronic or surgical wounds. Chlorhexidine is used in veterinary practice as well, in wound care and to treat infections of the mouth and ear. Regardless of how they are applied, though, all current chlorhexidine products suffer from the same limitation: the chlorhexidine salts used are highly soluble, meaning that when they are placed in a damp environment, the local liquids rapidly remove the chlorhexidine. For this reason, its activity is limited to a short period after application and it needs to be reapplied regularly, at relatively high concentrations, to provide any lasting protection.
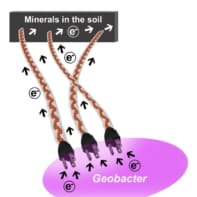
Our approach to this problem is a simple but very effective modification. By sequestering the chlorhexidine in salts of condensed phosphates, we create a material with much lower solubility, one that is stable when dry and that releases chlorhexidine at a steady (close to linear) rate in a wet environment. Naturally, given our background, our first thoughts were to exploit this new material in dentistry. The main cause of failure of modern dental fillings is secondary infection, where bacteria infiltrate the interface between the tooth and the filling material. By incorporating our sustained-efficacy chlorhexidine into the materials used at this interface, we can create a locally chlorhexidine-rich environment with a clinically optimal dose: sufficient to kill any microbes that penetrate, but not to adversely affect human cells. We can even incorporate a degree of “smart” behaviour, whereby the chlorhexidine release is accelerated in response to a fall in pH, which would indicate the very earliest stages of tooth decay in the area.
But of course, since chlorhexidine is also used widely in medicine and veterinary care, we have opportunities to exploit our technology in those areas as well. Although the material’s genesis was in a dental environment, our spin-out company Pertinax Pharma is now developing wound-dressing materials with a lasting antimicrobial effect for conditions such as burns and diabetic foot. The slow release of the antiseptic means that our prototypes do not elicit the adverse response from human cells associated with high doses of chlorhexidine and other antiseptics. We are also now developing a spray-delivery, resilient, water-resistant film of our material that could find applications in diverse fields. It could be used to prevent umbilical-cord infection in newborns, for example, especially in developing countries where the material’s low cost, long-term efficacy and benign storage requirements (with the consequent ease of transport) make it an appealing option. This material could also be used in an actual field, to treat infectious foot disease in cattle.
These are the applications I find the most exciting. There is a great deal of overuse and misuse of antibiotics, and although reducing this (and managing or combatting the antibiotic resistance that results from it) will require a multidisciplinary approach, the development of technologies such as ours – which can be used in place of antibiotics to give a clinically equal or superior outcome – can certainly play a part. I hope to see materials such as our novel chlorhexidine salts make a substantive difference to the global community not only via innovative dental materials that can protect against tooth decay, but in the wider fields of medicine and dentistry where sustained-efficacy antiseptics can serve a multitude of purposes.
- Enjoy the rest of the 2018 Physics World Focus on Biomedical Physics in our digital magazine or via the Physics World app for any iOS or Android smartphone or tablet.