To improve the accuracy of proton therapy delivery, and therefore its effectiveness, the ability to verify proton range in the patient is highly beneficial. In vivo range verification would give confidence in reducing margins and be used as a trigger to detect any need for adaptation.
Prompt-gamma imaging (PGI) is one method being developed for in vivo range verification. An interdisciplinary team of researchers at OncoRay, the National Center for Radiation Research in Oncology in Dresden, successfully applied a prompt gamma camera developed by IBA in a proof-of-principle application in clinical treatments using double-scattered protons (see: Prompt gamma imaging goes clinical). A team at the University of Pennsylvania used a second such unit to record the first clinical treatments in pencil-beam scanning (PBS) mode (see First clinical prompt gamma imaging of PBS protons).
In a next step, Lena Nenoff from the translational research team at OncoRay has conducted a study to evaluate the sensitivity of the camera to detect different types of range shifts, beam delivery techniques and evaluation methods, in close-to-clinical scenarios. The researchers systematically assessed the performance of the slit camera in well-defined error scenarios using realistic treatment deliveries to an anthropomorphic head phantom (Radiother. Oncol. 125 534).
Detecting deviations
Range shift deviations occur for a variety of reasons. They can be caused by changes in patient anatomy, intra- and inter-fractional motion, and/or setup errors during each fraction. Range shifts also occur due to uncertainties in the nominal range prediction, mostly resulting from uncertainty in the conversion of CT numbers into stopping behaviour of particles (stopping power ratio), and/or from uncertainties in the beam model.
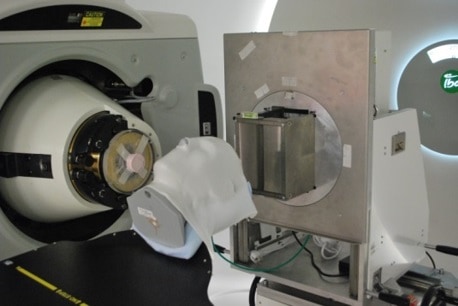
The PGI slit camera projects the prompt-gamma distribution through a knife-edge slit collimator onto a segmented detector, a geometry optimized in collaboration with Université Libre de Bruxelles. This results in a one-dimensional spatially resolved prompt-gamma distribution measured by extremely fast electronics (designed by partners at Politecnico di Milano and XGLab).

For the study, the authors defined a clinical target volume (142 cm3) representative of a brain tumour in the temporal lobe in a head phantom. They developed three treatment plans: double-scattering; a single-field uniform dose; and intensity-modulated proton therapy. The three plans consisted of two equally-weighted fields, only one of which was monitored by the slit camera.
In experiments performed at OncoRay’s clinical proton facility, the researchers positioned the slit camera next to the phantom, with the collimator opening parallel to the beam. The field-of-view was approximately 10 cm along the beam axis and focused on the distal part of the target volume. They introduced various local and global range shifts of known magnitude.
The accuracy of the PGI simulation was better than 1 mm. Deviations from the treatment plans were detected with an accuracy of better than 2 mm in PBS by comparing the measured PGI information with the expected PGI signal from the simulation. The researchers concluded that detection of global and local range shifts with a PGI slit-camera is possible under simulated clinical conditions. PGI verification of PBS was superior to verification of double-scattering.
Co-author Christian Richter, the senior researcher in the translation slit camera project at OncoRay, told medicalphysicsweb that an open clinical trial to identify the clinical benefit of prompt-gamma based range verification is underway at the University Medical Center Klinik und Poliklinik für Strahlentherapie in Dresden. The first patients where the researchers applied the slit camera during double-scattering treatments are included in the study, but it will primarily include patients who will be monitored with the slit camera during PBS treatments. PBS is becoming clinically available at the clinic in mid-December 2017, and patients will be actively recruited to participate. The OncoRay and IBA team are also currently working on an update of the camera trolley design, with the aim of extending the applicability to more clinical indications.



