How can the clinical potential of PET/MRI be unlocked? What challenges lie ahead? Cancer imaging expert Vicky Goh took out her crystal ball and provided some insight into the future role of PET/MRI and how both modalities can be integrated effectively. She also touched on PET/CT.
Why is the UK lagging behind other countries when it comes to PET/MRI? That was one of several questions she was asked after her keynote lecture during the British Institute of Radiology (BIR) annual congress, held virtually on 4 and 5 November.
Scanner numbers and the stance on evidence-based practice play a major part in its progress in this area, according to Goh, who is professor and chair of cancer imaging and head of the cancer imaging department at King’s College London.
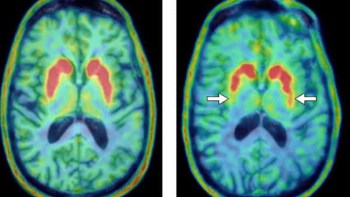
“We only have a handful of scanners in the country and the majority of those were funded through the Dementia Platform UK initiative. In terms of the neurology and neuro-oncology direction, we are probably further along, but we are still looking at PET/MRI as a clinical research tool,” she told attendees.
Goh, who received the Most Influential Radiology Researcher award in the inaugural EuroMinnies in 2019, said there needed to be changes in the “direction” of PET/MRI.
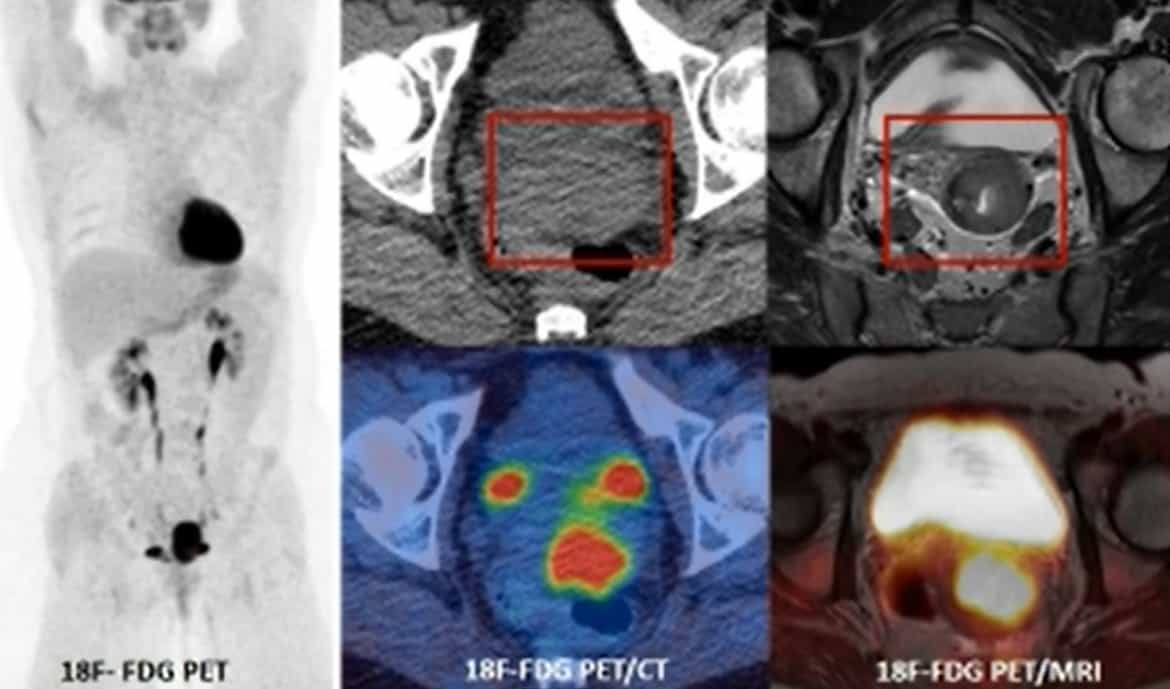
“We are very much an evidence-based practice and the evidence base is there for certain types of cancer. In prostate cancer you can see that prostate-specific membrane antigen (PSMA) PET/CT followed by targeted PET/MR would actually be of benefit to staging,” she explained.
“But the issues still remain: limited access, and limited dual-trained practices. In terms of outsourcing to other centres, a spoke and hub model will do quite well for referrals, but we need more scanners, we need more trained staff, and we need more evidence to push ahead in the UK with our practice.”
Evidence-based practice and AI
Given the need for evidence-backed protocols before wide-scale adoption and the lack of funding to provide PET/MRI in centres, Goh was asked by another online attendee how she envisaged the technique becoming widely adopted without significant delays.
Goh, who is also honorary consultant radiologist at Guy’s & St Thomas’ Hospital, noted that the only way was for institutions to work together and pool data and experience to get across the adoption gap in terms of data and protocols.
“Funding will always be an issue, but it’s one of those chicken-and-egg situations: the more data you have and the more utility you see, then the likelihood is that funding will increase,” she said. “It’s a case of ‘watch this space’, but in terms of cancer phenotyping and the type of radiologist that I want to be, there’s no doubt that this is one of the modalities I want to work with clinically.”
Goh was also asked if there is a role in the hybrid workflow for artificial intelligence (AI) systems.
She explained that in terms of improving prediction of prognostication, the data are still limited from research groups looking into this area, and larger datasets are needed. However, by improving noise and processing of the whole-body components there would be reduction in whole-body scan times, particularly for MRI diffusion scans.
“T1 and T2 scans are quick but it’s the diffusion we want to cut down to two or three minutes per station. It also means we can start looking at other things like segmentation, and quantitation in an automated fashion and again this is an area where we need to ‘watch this space’,” she said.
Clinical applications
Discussing myeloma treatment response with session chair and BIR president Sridhar Redla, Goh pointed to an exciting new role for PET/MRI. While MRI is the most sensitive modality for myeloma detection, there are, to date, more data for PET in the treatment response setting. PET-positive patients who show a reduction in PET uptake are more likely to do well and have a longer disease-free interval.
“What we really need is a modality that is both sensitive but also able to provide physiological information in the treatment response setting. And as a one-stop in this elderly population, we can offer them one examination [PET/MRI] rather than have them come back for three examinations (CT, whole-body MRI, then FDG-PET/CT) at multiple time points – in an elderly population this isn’t so viable. This is definitely one area where we can have a win,” she said.

Goh also discussed the advantages of whole-body pseudo CT, whereby MRI is used to develop a CT scan with Hounsfield units equivalent to a CT that is acquired in clinical practice.
This can then be leveraged to improve standardized uptake value (SUV) quantitation from bone, which is one of the issues with attenuation correction, she noted, as well as for radiotherapy planning in which there is an issue of dosing. Although it’s early days, she pointed to great potential for this technique for prostate radiotherapy planning and gynaecological cancers.
In response to another question from an online viewer, Goh noted that for small-volume lung disease, chest CT remained the standard detection tool. However, she pointed to developments in the MR sequencing that might change this in future.
PET/CT versus PET/MRI
Another listener wanted to know if patients with a strongly suspected cancer based on chest X-ray should go directly to PET/CT rather than CT first and then PET/CT. For those who are going to have definitive therapy – for lung or oesophageal cancer, for example – PET/CT should be the way forward, Goh answered. This is because these patients often have metastatic disease presentation and PET/CT is the most sensitive way to pick up this disease.
What about colorectal cancer? Whole-body MRI can detect a higher number of metastases than just contrast-enhanced CT can, she continued. For colorectal cancer and metastatic disease in sites such as liver, brain and bone, FDG PET/MRI improves detection, she added.
But, does PET/MRI pick up more liver lesions than PET/CT? Responding to this question from Redla about neuroendocrine cancers and somatostatin receptor imaging, Goh noted that the answer wasn’t straightforward, and due to complex protocols.
“As we all know, diffusion is the most sensitive sequence for picking up lesions, and it’s the diffusion component of the MR that is really contributing here in whole-body PET/MRI. We’re also able to pick up discrepancies, lesions that are tracer positive versus those that are tracer negative, to provide a more realistic burden of disease and the proportion of it that is potentially going to respond,” she noted. Small lesions that are receptor-negative will probably not respond to therapy, she clarified.
So with more resources, will PET/MRI replace PET/CT? Goh’s short answer was “no”. She pointed to certain scenarios where PET/MR can either complement PET/CT, as in prostate cancer staging, and others where PET/MR would replace it, as in the myeloma setting. But PET/CT was far quicker to perform than PET/MR and would keep its place in the clinic.
“Think about scheduling and the number of PET/CTs we ask for. The number of patients examined in a day would be phenomenally different. So we can’t see this replacing PET/CT except in certain scenarios but we can definitely see it complementing it,” she said.
- This article was originally published on AuntMinnieEurope.com ©2021 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.