
The curative potential of radiation therapy is limited by normal tissue toxicity, which restricts the dose that can be delivered to nearby non-target tissue. Recently, interest in ultrahigh dose rate radiotherapy has been rekindled, following preclinical studies showing increased normal tissue tolerance at high dose rates. This approach – known as FLASH radiotherapy – employs dose rates exceeding 40 Gy/s and can improve the therapeutic ratio by increasing the differential response between normal and tumour tissues.
The expectation is that FLASH could one day provide tumour ablation in a single sub-second treatment, while substantially reducing radiation-induced side-effects. The underlying mechanism, however, is not yet understood and requires further research. And to date, FLASH dose rates typically require specialized electron sources or substantial modifications to clinical linacs.
“Access to FLASH beamlines is limited and the progress on understanding of the FLASH mechanism is quite slow,” explains Magdalena Bazalova-Carter from the University of Victoria’s XCITE Lab. To remove this constraint, Bazalova-Carter and PhD student Nolan Esplen are investigating the feasibility of using a conventional high-powered X-ray tube for FLASH radiotherapy (Med. Phys. 10.1002/mp.13858).
“Our results will hopefully inspire researchers without access to high-power electron sources or proton beamlines to perform FLASH in vitro, and possibly some limited in vivo experiments, with a standard X-ray tube,” says Bazalova-Carter.”
The researchers used Monte Carlo (MC) modelling to evaluate the maximum dose rates achievable by two conventional X-ray tubes: the 3 kW MXR-160/22 (which was being validated in the XCITE lab) and the 6 kW MXR-165, which benefits from a short distance from the focal spot to the tube surface. For both tubes operating at maximum power, they simulated the output of an unfiltered 160 kV beam and calculated the dose deposited in a water phantom placed against the tube surface. They then converted the MC-calculated dose to dose rate.
The simulations revealed that both X-ray tubes were FLASH-capable, with maximum phantom surface dose-rates of 114.3 and 160.0 Gy/s, for the MXR-160/22 and MXR-165, respectively. Dose non-uniformity due to the heel effect – an inherent directional variation in the X-ray intensity emitted by the anode – was seen in both cases. For a 1 cm diameter region-of-interest within the high-dose region, dose rates were 110.6 Gy/s for the MXR-160/22 and 151.9 Gy/s for the MXR-165.
Plotting dose rate versus depth revealed a rapid fall-off for both 160 kV X-ray beams. At 2 mm depth, for example, dose rates decreased to 23% and 28% of that at the surface, for the MXR-160/22 and MXR-165, respectively. The dose rate remained FLASH-capable at depths of up to 1.4 and 2.1 mm, for the MXR-160/22 and MXR-165, respectively.
To validate their MC models, Bazalova-Carter and Esplen measured the dose in a plastic water phantom irradiated with a 120 kV beam from the MXR-160/22. They placed Gafchromic EBT3 films at 15 and 18 mm depth in the phantom and compared the measured 2D dose profiles with those from MC simulations of the 120 kV beam.
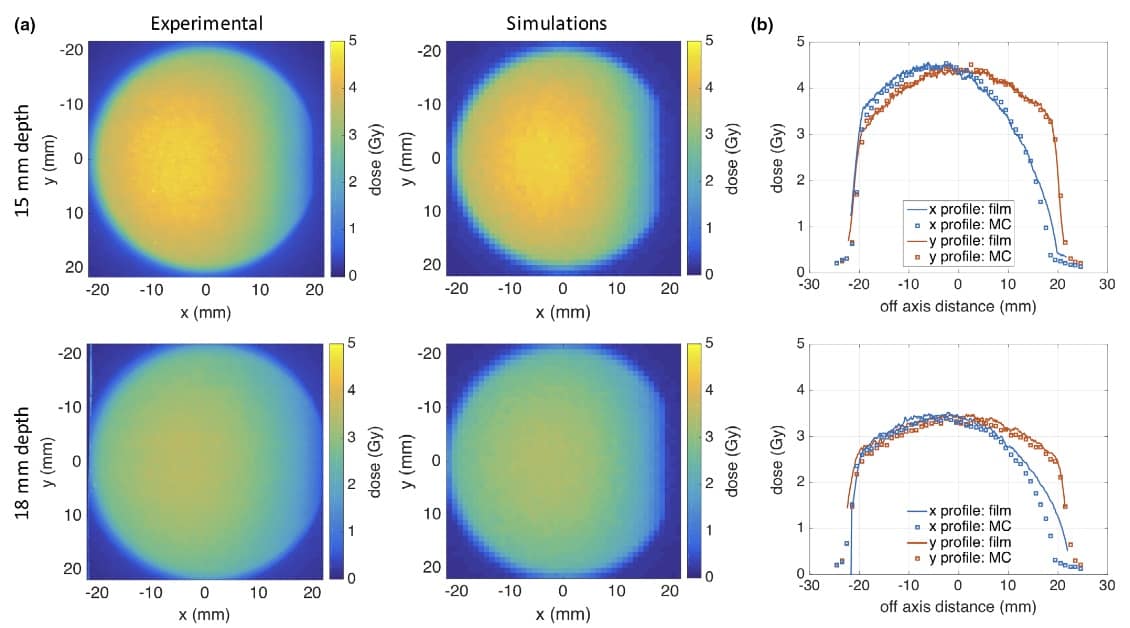
In the region not affected by the heel effect, the simulations agreed well with the film measurements. The mean X-profile differences between experiments and simulations were 1.5% and 3.2%, at 15 and 18 mm, respectively; the mean y-profile differences were 1.5% and 3.5%, at 15 and 18 mm. Agreement in the heel-effect region was poorer, however, with a mean difference of up to 17.8% along the X-profile.

FLASH radiotherapy: from preclinical promise to the first human treatment
This validation experiment demonstrates the ability of conventional X-ray tubes to deliver FLASH therapy. The researchers suggest that these particular tubes could be suitable for FLASH skin irradiations, in vitro experiments or testing dose-rate dependence of small-field dosimeters.
They are now working to further tailor the X-ray tubes for FLASH applications. “We are currently building a shutter mechanism that will inset in the X-ray tube, which will further increase the dose rate,” Bazalova-Carter tells Physics World. “We are also designing experiments to test cell survival for FLASH irradiations with and without gold nanoparticles.”



