How can technology developed at CERN for high-energy physics bring state-of-the-art radiotherapy to a hospital just along the lakeside in Lausanne?
The technologies in question include high-performance electron accelerator components and simulation tools originally designed for CERN’s Compact Linear Collider (CLIC). Now, a collaboration between CERN and Lausanne University Hospital (CHUV) plans to use these to create a system for clinical delivery of FLASH radiotherapy.
FLASH radiotherapy, which involves delivering therapeutic radiation at ultrahigh dose rates of 40 Gy/s and above, vastly decreases normal tissue toxicity while maintaining anti-tumour activity. Of particular note, FLASH should enable dose escalation, potentially offering a new option for cancers that are resistant to treatment. “In all experiments so far, we observed that normal tissues are spared with this type of radiation,” says Jean Bourhis, head of radiation oncology at CHUV. “It’s a really reproducible effect. And there is no sparing of the tumour.”
Bourhis pioneered the development of FLASH radiotherapy, leading the team at CHUV that performed the first FLASH treatment in a human patient in 2018. The patient in question had a resistant superficial skin cancer and was treated with low-energy electrons of roughly 10 MeV. Next, he would like to translate the impressive observations seen in an experimental setting into clinical trials. To treat larger tumours at depths of up to 20 cm in the patient, however, will require much higher energy electron beams.

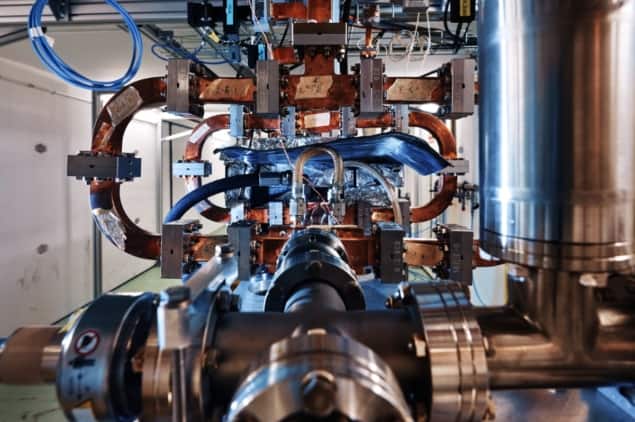
“A clinical FLASH system must have a high accelerating gradient to achieve the beam energies needed to access deeper-seated tumours, energies in the range of 100 MeV,” explains Walter Wuensch, a senior researcher at CERN. This ability to accelerate beams in a very short distance, he notes, was one of the technologies designed for CLIC. The other key aspect of the high-energy physics study was to deliver a high current in a well-controlled and extremely stable beam – another important requirement for FLASH.
“For some years, CERN has been studying accelerator technology for a possible high-energy physics facility,” says Wuensch. “We have developed prototypes and shown their feasibility and performance. So it was with real excitement that we found out about the needs of CHUV. After some initial discussions it became clear that what we had developed for CLIC seemed an almost perfect match for what is needed for a FLASH facility.”
“The clinical need that we have really converges with the technological answer that CERN has,” adds Bourhis. “This is really powerful.”
The CERN–CHUV partnership has now finished the first phase of its study: moving from an initial idea to creating a conceptual design for the proposed FLASH facility. The next step will be to develop this baseline design in more detail to optimize the system for patient treatments. The team also hopes to collaborate with an industry partner in the radiotherapy field. Alongside, while the machine is being prepared, CHUV will start to prepare the required teams and infrastructure, and submit applications to regulatory agencies so that the treatment can reach patients as soon as possible.
Bourhis predicts that the FLASH facility should be operational within two to three years, at which point the team plans to embark on proof-of-concept in clinical trials. He notes that after these trials, the system could be transferable to other hospitals.

FLASH radiotherapy: from preclinical promise to the first human treatment
The system will be 2–2.5 times larger than a conventional radiotherapy machine, but should still be compact enough to fit into existing hospital infrastructure. The cost of the first protoype system (being installed in CHUV) is estimated to be about €25m; though if manufacturing scales up, this price should come down. FLASH treatments, however, only require the patient to undergo two or three radiation fractions, compared with 20 or 30 for standard radiotherapy. As such, Wuensch suggests that the eventual cost-per-treatment could be competitive in absolute terms with classical radiotherapy.
“We really appreciate the opportunity to work on something that’s matches so well and is new on both sides,” Wuensch concludes. “It’s a wonderful opportunity to be able to work in the medical field.”



