Molecular radiation therapy (MRT) is a treatment in which radioisotopes given orally or intravenously are used to deliver radiation to diseased tissue. As with all radiotherapy techniques, successful treatment relies on accurate control of the dose to the target. But in contrast to external-beam irradiation, with MRT it is not possible to accurately plan the delivered dose, due to the lack of control over the uptake, retention and distribution of the radioisotope within tissue.
As such, there’s a real need for patient-specific dosimetry to assess the dose delivered to the treated tissue. Currently, however, MRT dosimetry techniques are limited. Addressing this shortfall, research led by the University of Surrey investigates whether measurements of Cherenkov light at the patient surface could be used for a new MRT dosimetry technique.
Cherenkov light is produced in tissue when charged particles travel at a speed greater than the phase velocity of light in tissue. In MRT, charged particles are created as the administered radioisotope decays. All of these charged particles deliver therapeutic dose, while only those with high enough phase velocity also produce Cherenkov light.
The relationship between the dose delivered to the tissue and the emitted Cherenkov light intensity is linear – a necessity for dosimetry based on Cherenkov light. Other requirements include a small inter-patient variability in this linear relationship and ensuring that the measured optical signal probes the treatment volume.
In a study reported in Biomedical Optics Express, the researchers investigated the effect of inter-patient variability in tissue characteristics and radioisotope uptake on the linear relationship between the dose absorbed by the treatment volume and Cherenkov light intensity at the surface of the patient.
“Our study showed how the spatial and spectral characteristics of Cherenkov light can be exploited to optimize the performance of a Cherenkov-based dosimetry technique,” explains first author Jigar Dubal from the University of Surrey.
Numerical experiments
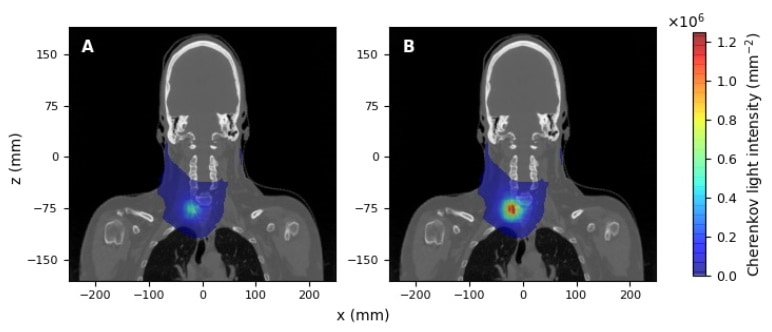
Dubal and colleagues simulated MRT using iodine-131 (131I), as employed clinically, to treat hyperthyroidism and papillary thyroid carcinoma (PTC). This radioisotope undergoes beta decay, producing electrons that deposit dose and generate Cherenkov light. They used clinical CT images to create the 3D patient geometry, with tissue types defined by the densities obtained from the CT scanner calibration curve. To model the light emission and propagation within the patient, they assigned optical parameters to each tissue type, and considered the inter-patient variability in these characteristics.
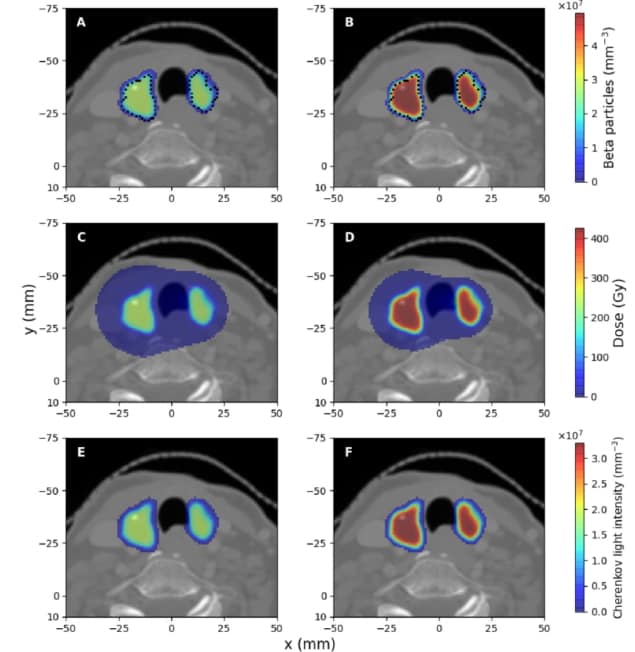
For hyperthyroidism, the simulations considered 131I spread throughout the thyroid gland. For PTC, the radioisotope was either distributed solely in the tumour or with some accumulation also in surrounding thyroid tissue, thus modelling the patient variability in radioisotope distribution. The team simulated 131I decay within the treatment volume to determine the spatial distribution of the beta particles, the deposited dose and the spectral and spatial characteristics of the Cherenkov light.
The simulations showed that the emitted Cherenkov light was localized in the treatment volume, with the light distribution mostly overlapping with deposited dose. While the light intensity varies linearly with the absorbed dose, this relationship is patient-specific, due to differences in patients’ tissue optical properties and, in the PTC case, radioisotope uptake.
The team next assessed the Cherenkov light emerging at the patient surface, which could be measured for dosimetry applications. In this study, while Cherenkov light is mostly emitted at lower wavelengths, simulations showed that surface light is predominantly in the near-infrared (where tissue absorption is minimal). In this spectral range, the Cherenkov light reaching the surface mostly originates in the treatment volume, and its spatial distribution exhibits areas of high intensity, dependent upon the position and symmetry of the treatment volume
The researchers also examined the relationship between the mean dose deposited in the target and the total Cherenkov light intensity, for measurements over the entire surface area and in a 25 x 25 mm hot spot. They demonstrated that the relationship between dose and light intensity was more robust to inter-patient variability (in tissue optical parameters and radioisotope uptake) when light was measured at the hot spot rather than over the whole surface, and more robust for PTC treatments than for hyperthyroidism treatments.

Visualizing the treatment beam improves radiation therapy delivery
These findings could pave the way for patient-specific MRT dosimetry based on Cherenkov light measurements. To optimize the accuracy in estimating the mean dose deposited in the treated volume, the researchers recommend surface light measurements in the near-infrared spectral range and at the intensity hot spot on the surface
While inter-patient variability affects the dosimetry accuracy, the researchers note that the uncertainty in estimating the dose using Cherenkov light can be less than for current MRT dosimetry methods.
The team is continuing numerical experiments with the aim of devising a 3D dosimetry technique. “Using Cherenkov light could provide a more accurate and cost-effective alternative to existing dosimetry techniques for molecular radiation therapy,” says senior author Lucia Florescu. “We are currently considering utilizing multiple surface light measurements to reconstruct the 3D Cherenkov light distribution within the tissue, to gain insight about the 3D dose distribution and achieve comprehensive patient-specific dosimetry.



