FLASH radiotherapy, delivered using ultrahigh-dose-rate (UHDR) radiation beams, can significantly reduce normal tissue toxicity while maintaining anti-tumour efficacy. Preclinical studies demonstrating this FLASH effect have mostly employed electrons and protons, as it is relatively easy to generate UHDR beams by adapting existing medical accelerators. But to translate FLASH for use in patients, the high-energy (megavoltage) X-rays commonly used in conventional clinical radiotherapy could provide a more optimal approach.
With this in mind, a research team headed up at Tsinghua University in China is developing a FLASH radiotherapy platform based on a room-temperature RF linear accelerator (linac) – as widely used in medical applications due to its compact size and low cost. They demonstrated that their system, described in Medical Physics, can produce high-energy X-ray beams with a dose rate exceeding 40 Gy/s in a clinically relevant set-up.
“The potential advantages of using X-rays in FLASH radiotherapy are the compactness of the machine and high cost-effectiveness of the treatment,” researcher Hao Zha tells Physics World. “The length of our accelerator was only 1.65 m, so the experiment could be installed in a small room.”
Accelerator optimization
High-energy clinical X-ray radiotherapy systems are typically based on a room-temperature RF linac that accelerates electron beams to the MeV level. These electrons then irradiate a target that converts them into high-energy X-rays via the bremsstrahlung effect. The achievable X-ray dose rate depends upon both the energy and current of the incident electron beam.
FLASH radiotherapy, however, requires a dose rate 2–3 orders of magnitude higher than that of conventional systems. In this study, the team achieved this by increasing the mean beam current from tens of microamperes to several milliamperes.
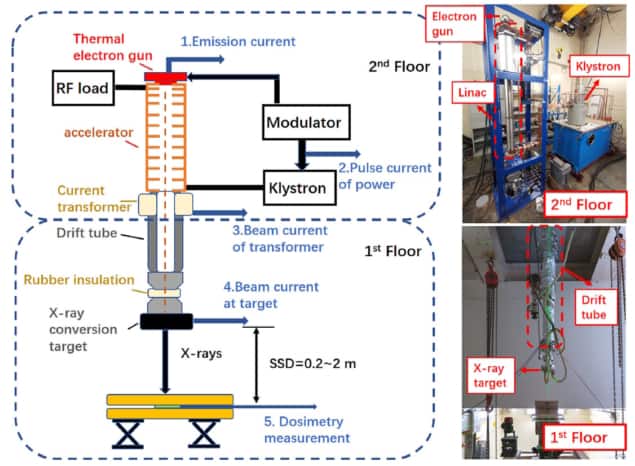
Zha and colleagues developed their UHDR high-energy X-ray radiation platform by optimizing an S-band backward-travelling wave electron linac. They designed a 1.65 m-long accelerator that uses a klystron-based power source to generate 11 MeV electron beams with a pulse current of 300 mA, a 12.5 µs pulse length and a mean beam power of 29 kW.
The next obstacle is that such high-mean-power electron beams deposit vast amounts of heat in the electron-to-photon conversion target. To help mitigate this heating, the team sent the electron beams through a 1.8 m-long drift tube that increased the transverse beam size from 5.1 to 10.6 mm, thereby decreasing the power density and pulse heating at the target.
The performance of the conversion target, which comprises a tungsten disc as the functional area surrounded by copper to enable water cooling, is dependent upon the thicknesses of tungsten and copper in the beamline. Thus the researchers used Monte Carlo and thermal finite element analysis simulations to optimize the material thicknesses.
Modelling 1.4–4 mm of tungsten and 1.5–3 mm of copper revealed that the X-ray dose rate decreased with increasing thickness of either material. To maximize X-ray conversion efficiency while maintaining safe cooling, they created a target with 3 mm tungsten and 2 mm copper. This combination could produce pulsed X-rays with a mean energy of 1.66 MeV and a dose rate of 40.2 Gy/s at a source–surface distance (SSD) of 70 cm in simulations.
Linac dosimetry
To assess the performance of their room-temperature linac, the researchers used EBT3 and EBT-XD radiochromic films to perform absolute dose measurements. They placed the films 50 or 67.9 cm from the X-ray target, at 2.1 cm depth in a water phantom. The maximum mean dose rates exceeded 80 Gy/s at 50 cm SSD and 45 Gy/s at 67.9 cm SSD, with good agreement between the two film types.
The researchers also used a PTW Farmer-type ionization chamber at 100 cm SSD to measure the relative total dose of each radiation shot, and a plane-parallel ionization chamber placed under the film to measure the relative dose of each pulse. The mean steady state dose rate (calibrated with the film results) was 49.2 Gy/s at 67.9 cm SSD. Pulse and bunch dose rates were 5.62 and 59.0 kGy/s, respectively.
The team also used the plane-parallel detector to test the system stability. The standard deviation of 20 consecutive radiation shots was 1.3% of the total dose. By changing the irradiation control strategy, the researchers improved this shot-to-shot dose stability to 0.3%. The day-to-day stability had a poorer standard deviation of 3.9% over 70 radiation shots (10 per day for seven days) – attributed to daily temperature changes.
The researchers note that the linac system can produce both UHDR and conventional irradiation without any changes to the platform setup. The mean dose rate can be adjusted by changing the pulse repetition rate (from 1 to 700 Hz) and pulse length (from 6.3 to 12.5 µs). In addition, the mean dose rate and pulse dose rate can both be adjusted by changing the SSD of the platform.
High-energy physics devices adapted for electron FLASH dosimetry
In future implementations, they suggest, the static conversion target could be replaced with a rotating design. This would help reduce the burden on the cooling system and remove the need for the beam expansion drift tube, further increasing the system’s compactness and simplicity.
“The results are encouraging for future work to introduce X-ray FLASH radiotherapy based on room-temperature linacs into clinical applications,” the researchers conclude. “Because it has the advantages of affordable cost, system simplicity and a compactness suitable for most hospital treatment rooms, the room-temperature linac system is proposed to be a competitive FLASH radiotherapy solution with considerable appeal.”



