Researchers from Dartmouth have developed a method to convert a standard clinical linear accelerator (linac) used for radiation therapy to deliver a FLASH-capable, ultrahigh-dose rate (UHDR) radiotherapy beam. The process, which uses existing accessories, takes only 20 minutes to perform, or to reverse.
UHDR radiotherapy delivers radiation at dose rates that are hundreds, or even thousands, times higher than used in conventional treatments, leading to a phenomenon commonly referred to as the FLASH effect. Adapting a linac to deliver radiation at 300 Gy/s rather than 0.1 Gy/s enables treatment to be completed in 6 ms instead of 20 s. Crucially, preclinical research with laboratory animals has shown that these high dose rates significantly reduce toxicities to surrounding healthy tissue while maintaining anti-tumour activity.
“We believe this is the first reversible UHDR beam on a clinically used linac where the beam can be used in the conventional geometry where patients are on the treatment couch,” says Brian Pogue, of the Thayer School of Engineering and the Norris Cotton Cancer Center.
Writing in the International Journal of Radiation Oncology, Biology, Physics, Pogue and colleagues describe the procedures and guidelines that they developed to deliver UHDR to a treatment room isocentre.
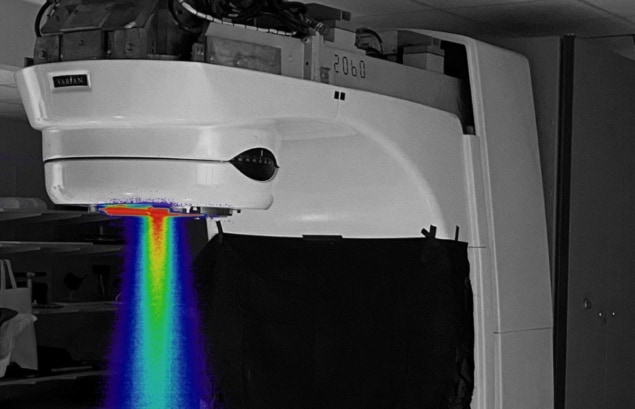
The team converted a Varian Clinac 2100 C/D to deliver UHDR electron beams using existing accessories including jaws, applicators and cutouts. The conversion was performed by setting the treatment console to “service mode” and manually resetting some key components of the treatment delivery system – the carousel, air valve and target – with the gantry angle set at 90 degrees to access these components.
Modifications (which could be completed within 20 minutes) included retracting the X-ray target and flattening filter from the beam’s path, positioning the carousel on an empty port and selecting 10 MV photon beam energy in the treatment console to deliver electron beams. To convert the linac back for conventional radiotherapy use, this process is simply reversed.
Following the conversion, the researchers used film and an optically stimulated luminescent dosimeter (OSLD) to measure dose-rate, surface and depth–dose profiles in solid water phantoms. They used a fast photomultiplier tube-based Cherenkov detector to measure per pulse beam output at a 2 ns sampling rate.
FLASH accomplished
Lead authors Mahbubur Rahman and Ramish Ashraf of the Thayer School of Engineering and colleagues report that the converted system could achieve dose rates of up to 290±5 Gy/s at the isocentre (100 cm source-to-surface distance), well above the reported 40 Gy/s threshold needed to potentially achieve the FLASH effect. The doses measured from simultaneous irradiation of film and OSLD agreed to within 1%. The radial symmetry of the beams was within 0.2% at 290 Gy/s. The Cherenkov detector showed that the linac required a ramp-up period for the first 4–6 pulses before the output stabilized to a stability within 3%.
Based on these findings, the researchers believe that with further tuning of the beam output and reduced source-to-surface distance, they could achieve dose rates of up to 600 Gy/s. The variability of the radiation dose from the first few pulses may require a dose monitoring and stopping system for future clinical translation studies, and upwards of 10 pulses may be needed when performing preclinical animal investigations. Work is underway to develop a low-cost translatable controller circuit that could be used with the converted linac.
The researchers are currently using the UHDR beam in preclinical studies on experimental animal tumours, as well as in clinical veterinary treatments. Murine studies are underway to examine the nature of the normal tissue sparing from radiation damage that the FLASH effect confers. Veterinary treatments to dogs with sarcoma tumours are being used to test out the ability to safely deliver this beam.
“Further oxygen consumption from the FLASH beam has been widely postulated to be one of the factors that could lead to the FLASH effect of normal tissue damage reduction, and so, in vivo studies of this effect are being completed,” Pogue tells Physics World.
“Additionally, radiation oncologists and dermatologists have joined the team to design a human safety clinical trial using FLASH radiotherapy to treat patients with advanced skin lesions that cannot be surgically removed,” he adds. “There are a number of advanced lesions where, because of poor perfusion or lesion location, surgical removal would not be ideal. These might be better treated by radiotherapy, especially if there is a slightly enhanced sparing of the normal skin from the FLASH effect. The team is planning for this future trial to evaluate the safety of UHDR delivery in human treatment.”



