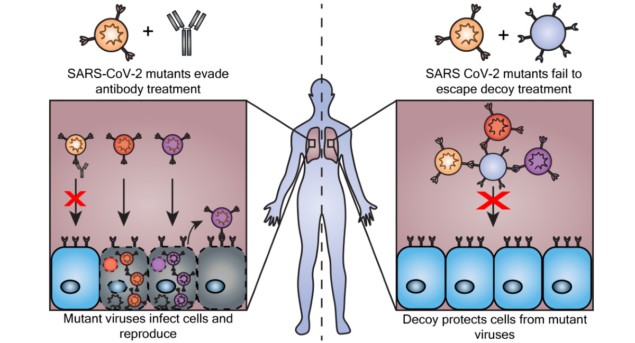
The ACE2 protein is the cellular door through which SARS-CoV-2, the virus that causes COVID-19, enters cells. What if we could trick SARS-CoV-2 into binding to decoy cells that render the virus inactive?
Nanoparticles may be the answer. By binding their ACE2 receptors to viral spike proteins, nanoparticles could act as cellular decoys that soak up viral particles like a sponge.
Cellular decoys soak up SARS-CoV-2
Scientists were testing the effectiveness of nanoparticle decoys for blocking viral infection before the COVID-19 pandemic even began. Such decoy nanoparticles are custom-built extracellular vesicles. Part of our body’s natural transit system that carries cargo between cells, extracellular vesicles are roughly the size of viral particles and about 10 million times smaller than human cells.
Researchers at Northwestern University had lingering questions about the nanoparticles’ effectiveness against SARS-CoV-2 and its variants, such as Delta and Omicron, that they wanted to answer before moving this potential therapy to in vivo animal studies and clinical trials. Their resulting experiments, published in the journal Small, shed light on what the nanoparticles require (or do not require, as the case may be) to be effective against SARS-CoV-2 infection.
“What we didn’t know was how to design and ultimately manufacture [nanoparticles] in a way that specifically prevents viral infection in the context of a rapidly evolving virus,” says Northwestern synthetic biology and engineering professor Joshua Leonard. “That was the focus of our study.”
Leonard and co-senior author Neha Kamat wanted to know which nanoparticles were most effective at trapping SARS-CoV-2 and its variants. To find out, they designed and manufactured various nanoparticles, each with 500 to 2000 ACE2 molecules. SARS-CoV-2 readily bound to these ACE2-bearing nanoparticles. Overall, the nanoparticles were up to 50 times more effective at inhibiting naturally occurring SARS-CoV-2 mutants when compared with soluble recombinant ACE2, which is similar to antibody drugs that are also recombinant proteins.
A new therapy, a rapidly evolving virus
Through this study, the scientific community may have a better understanding of how nanoparticle decoys perform against emerging viral strains. The nanoparticles were effective against several SARS-CoV-2 variants, including Delta and Beta. Results didn’t depend on which manufacturing method was used to create the nanoparticles. When the researchers tested the nanoparticles against a viral mutant designed to resist treatment, the decoys were up to 1500 times more effective at inhibiting infection than soluble recombinant ACE2.
Kamat and Leonard credit graduate student Taylor Gunnels with the conception and execution of these experiments. Gunnels, who is first author on the paper, leveraged the expertise of Kamat’s and Leonard’s labs to engineer the nanoparticles and test them against different SARS-CoV-2 variants.
“As we were conducting the study, different variants kept popping up around the world,” Kamat said in a Northwestern press release last month. “We kept testing our decoys against the new variants, and they just kept working.”

Cellular nanosponges could neutralize SARS-CoV-2
Now, the team is looking to understand how the decoys block infection. Also requiring study is how nanoparticles function in vivo and how the human body would remove or recycle a decoy-virion complex. Once these concepts are better understood, the researchers say that the nanoparticle therapy could be used to treat patients with severe disease or immunocompromised people who react poorly to other therapies.
“We’ve been gratified to see the excitement generated around the general strategy of using decoy particles for treating COVID-19 and maybe other viral infections,” Leonard says. “We hope that such knowledge could have a lot of utility in the early stages of a future pandemic before suitable drugs and vaccines are developed.”