Drug-infused microneedles that dissolve upon insertion could make photodynamic therapy (PDT) more effective at treating skin cancers, according to a study in the Journal of Biophotonics.
Microneedle developers from Queen’s University Belfast and PDT researchers from the University of São Paulo fabricated arrays of 500-µm-long needles by mixing a water-soluble polymer and a precursor to a PDT photosensitizer. In experiments with mice, these dissolving microneedles proved better than topical cream-based administration – the conventional approach for PDT – at delivering the therapeutic agent to a tumour’s surface. The researchers say that the results are especially promising for the treatment of thicker skin lesions.
PDT works on the principle that certain chemicals that are innately non-toxic can be “activated” when irradiated with the right frequency of light. When this happens, these photosensitizing chemicals convert molecular oxygen in the surrounding tissue into reactive species, which damage nearby cells. By shining the light only on the tumour, clinicians can target cancerous cells while sparing adjacent healthy tissue.
The challenge in applying this technique lies in getting the photosensitizer to where it can have the greatest effect. Michelle Barreto Requena, at the University of São Paulo, and colleagues adopted a commonly used solution to this problem in that they delivered not the photosensitizer itself, but its precursor, aminolevulinic acid (ALA).
ALA is a naturally occurring metabolite involved in the biosynthesis of haem. When an external supply of ALA is introduced, the chemical is taken into cells, where it is processed to form the photosensitizer protoporphyrin IX (PPIX). Although this produces the required therapeutic levels of PPIX in the intracellular environment, applying ALA as a cream means that only the more superficial cells of the tumour are treated. This is the limitation that Requena and colleagues sought to overcome with their dissolving microneedles.
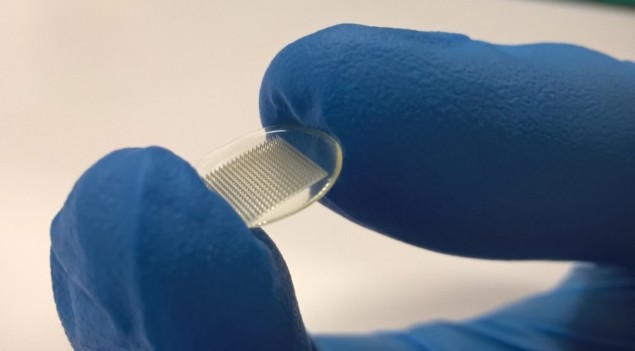
The team created their ALA microneedles by mixing the precursor with a combination of methyl vinyl ether and maleic anhydride. Shaping and drying the mixture in silicone moulds yielded arrays of microneedles hosted on square patches about 7 mm across. Each array’s 361 needles were 500 µm long, 300 µm wide at the base, and were spaced 50 µm apart.
To investigate the effectiveness of the microneedle arrays, the researchers tested them on live mice in which skin cancers had been induced. They secured the arrays against the animals’ lesions using tape, then waited 60 min for the ALA to penetrate the cancerous tissue and be converted to PPIX. They then measured the concentration of PPIX in the live animals using widefield fluorescence imaging and fluorescence spectroscopy. After the mice had been euthanized, the team measured the distribution of PPIX with depth using fluorescence confocal microscopy.
Compared with animals in which ALA had been delivered topically as a cream, the mice treated with microneedle arrays exhibited a 200% increase in mean PPIX fluorescence intensity according to spectroscopy analysis, indicating a much greater uptake of the precursor. Fluorescence microscopy of the tumour sections also showed that the microneedles produced diffuse distributions of PPIX down to depths of around 0.5 mm, whereas the cream concentrated the photosensitizer at the lesions’ surfaces.
As well as achieving greater penetration than conventional cream-based PDT, treatments based on dissolving microneedles could be more cost-effective, because they don’t need such high concentrations of ALA. They could also lead to shorter procedures, as ALA delivered at depth is absorbed more quickly. Given these benefits, the researchers are hopeful that their technique could extend access to skin-cancer treatment, and that it could be rolled out soon.
“Due to its low cost and simplicity, our approach may fit in many countries that need to increase the availability of treatment for the population,” says Requena. “There are always optimization studies that can be explored, such as decreasing the time for the dissolution of the microneedles. However, with these very promising results, we believe that this technology is potentially ready to be explored in clinical studies.”