
Reduced-dose dual-layer spectral CT (DLCT) is feasible in routine practice, despite the required higher tube potential, researchers from Heidelberg University Hospital, Germany, reported in a study published in European Radiology.
DLCT can deliver comparable objective and subjective image quality to that of reduced-dose single-layer CT (SLCT), reported Thuy Duong Do, senior physician at the Clinic for Diagnostic and Interventional Radiology, and colleagues. Also, further dose reduction in the thorax might be possible by adjusting mAs thresholds.
Conventional CT acquires images in a single broad energy band, but spectral CT separates energy into two or more narrow energy bands. Because different types of energies are absorbed differently by tissues, they can provide insights into the different chemical compositions of tissues.
“DLCT acquisitions allow material decomposition (virtual non-contrast, iodine-only imaging and effective atomic numbers) as well as the calculation of virtual monoenergetic images,” noted the authors, adding that several clinical studies have shown the benefits of DLCT for head CT to image intracerebral lesions and haemorrhage, for thoracic CT, for vertebral CT to differentiate bone lesions, and for abdominal CT angiographies to improve delineation of visceral arteries.
“For the image acquisition of such data, a tube potential of either 140 kVp or 120 kVp is necessary to allow for spectral decomposition under the exploitation of the energy-specific X-ray absorption of different materials,” they explained. “In contrast to changes in tube current, changes in tube potential have a nonlinear effect on radiation dose.”
Study details
The Heidelberg group’s overall aim was to quantitatively and qualitatively evaluate image quality in DLCT compared with SLCT in the thorax, abdomen and pelvis in a reduced-dose setting.
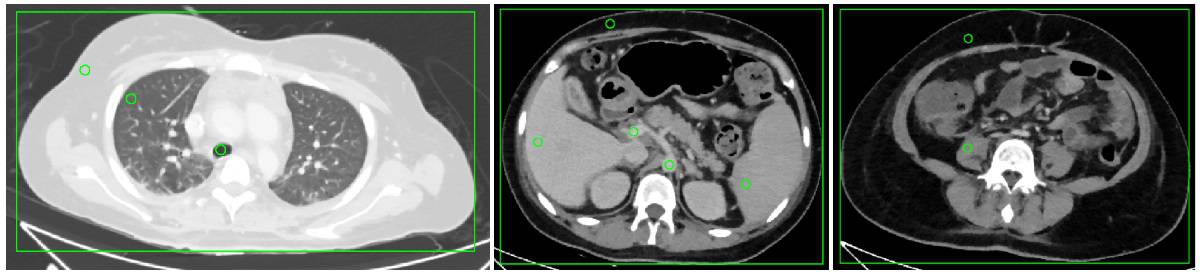
The researchers performed intra-individual, retrospective comparisons in 25 patients who received at least one acquisition of all three acquisition protocols – SLCTlow (100 kVp, iCT, Philips Healthcare), DLCTlow (120 kVp) and DLCThigh (120 kVp, IQon Spectral CT, Philips Healthcare) – covering the venous-phase thorax, abdomen and pelvis with matched volumetric CT dose index between SLCTlow and DLCTlow.
All examinations were conducted in the craniocaudal direction and supine position, with automatic exposure control, using an iohexol contrast agent (Accupaque 350, GE Healthcare). Contrast agent application was performed using a power injector with an injection rate of 3 ml/s.
Reconstruction parameters were identical for every scan. Image quality was assessed quantitatively at 10 measurement locations in the thorax, abdomen and pelvis by two independent observers, and subjectively with an intraindividual forced-choice test between the three acquisitions. The authors extracted dose–length product (DLP) and volumetric CT dose index (CTDIvol) for dose comparison.
The main findings were as follows:
- Despite matched CTDIvol in acquisition protocols, CTDIvol and DLP were lower for SLCTlow compared with DLCTlow and DLCThigh (DLP of 408.58, 444.68, 647.08 mGy·cm, respectively; p < 0.0004), as automated tube current modulation for DLCTlow reached the lower limit in the thorax (mean 66.1 mAs vs limit 65 mAs).
- Noise and contrast-to-noise ratio (CNR) were comparable between SLCTlow and DLCTlow (p values, 0.29–0.51 and 0.05–0.20), but CT numbers were significantly higher for organs and vessels in the upper abdomen for SLCTlow compared with DLCTlow. DLCThigh had significantly better image quality (noise and CNR). Subjective image quality was superior for DLCThigh, but no difference was found between SLCTlow and DLCTlow.
- DLCTlow showed comparable image quality to SLCTlow, with the additional possibility of spectral postprocessing. Further dose reduction seems possible by decreasing the lower limit of the tube current for the thorax, the researchers noted.
The team was surprised to see that the transition from 100 kVp to 120 kVp tube potential worked out so well in terms of both image quality and patient radiation exposure, according to corresponding author Stephan Skornitzke, a medical physicist at Heidelberg University Hospital.
“I would have expected that we would lose some contrast with the increase in tube potential, but the contrast-to-noise ratio turned out to be very similar before and after the switch to the new scanner and new protocol,” he told AuntMinnieEurope.com in an email. “Another surprise for me was to see how well the automatic exposure control is able to adjust the tube output to the patient anatomy.”
For the 120 kVp protocols, the exposure control hit the lower threshold for the tube current–time product in the thorax for a number of patients, where it wanted to regulate even lower but could not, he continued.
“This shows us that we can still optimize our acquisition protocols with an attention to detail and reduce patient radiation exposure,” Skornitzke explained. “The automatic exposure control was hitting the lower threshold for the tube current–time product in the thorax for a number of patients. We are in the process of evaluating an adjustment of this lower threshold, which may allow to further reduce patient radiation exposure, especially in smaller patients. However, we will have to carefully consider any potential impact on diagnostic image quality.”
Looking to the future
For follow-up studies based on the spectral imaging capabilities of the CT scanner, the researchers are investigating the potential clinical benefit of the large number of available spectral postprocessing applications. For example, they are evaluating calcium-suppressed imaging, which could allow for more accurate evaluation of bone marrow and fractures.
Also, they are planning to further investigate the connection between automated exposure control, image quality and patient radiation exposure.
“In the context of appropriate imaging, the automated exposure control is a very important tool, as it serves to ensure that the radiation is applied exactly where it is needed,” Skornitzke noted. “Today, with 3D-modulation, online-adaption and specific technologies like ‘Liver Boost’, we have a large number of methods available that help us to guarantee adequate image throughout the scan.”
More research is necessary to evaluate the complex interaction between these technologies, radiation exposure, and image quality, he stated.
The COVID-19 pandemic has provided new challenges for the radiological community regarding the fast and reliable assessment of the associated changes in the lung, and the Heidelberg group is involved in the research of these topics.
“Of course, the pandemic has affected all of our lives. However, as researchers in radiology, we are in a comparatively privileged situation, where our research often involves only a small number of people and a lot of work can be performed digitally, so that our research has so far only been affected minimally,” Skornitzke pointed out.
- This article was originally published on AuntMinnieEurope.com ©2020 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.



